Commercial Tobacco Prevention and Control
Tobacco Topics
- Behavioral Health
- E-cigarettes and Vapes
- E-cigarette School Toolkit
- Flavored Tobacco
- Menthol Tobacco
- Nicotine
- Quitting Tobacco
- JUUL Settlement
- Helping People Quit
- Secondhand Smoke
- Tobacco and COVID-19
- Tobacco 21
- Tobacco Taxes
- Traditional Tobacco
Related Topics
Contact Info
Commercial Tobacco Prevention and Control
Commercial tobacco use is still a problem. It kills over 6,300 Minnesotans every year and costs Minnesota $3.2 billion annually in medical costs. Investing in commercial tobacco use prevention and control saves lives and taxpayer dollars. We're working to reduce commercial tobacco's harm by:
- Reducing youth access to commercial tobacco.
- Reducing secondhand smoke exposure.
- Increasing access to cessation resources.
- Addressing commercial tobacco-related disparities.
Recent news
Now Open: Request for Proposals for Marketing Services
The Minnesota Department of Health requests proposals for a contractor to manage the brand identity for Quit Partner, Minnesota’s statewide commercial tobacco cessation service, as well as a promotional campaign to raise awareness of the service and encourage its use among Minnesotans who use commercial tobacco products, as authorized by Minnesota Statute 144.397: Statewide Tobacco Cessation Services. The 2019 Minnesota Legislature dedicated funding for the implementation of statewide tobacco cessation services to offer Minnesotans help in quitting commercial tobacco use.
Key Dates
- Posted: April 1, 2024
- Proposals Due: May 8, 2024 by 4 p.m.
Proposal Submission
The full solicitation is available in the state Supplier Portal. To view this solicitation, log into the Supplier Portal and search for Event ID 2000015631.
All required forms are available in the Supplier Portal.
Questions and answers
Questions may sent to Megan Kettunen, Finance Manager, at megan.kettunen@state.mn.us. Other personnel are not authorized to answer questions regarding this Solicitation.
Questions must be received by 4 p.m. on April 12, 2024. Questions and answers will be posted in the Supplier Portal by April 17, 2024, at 5 p.m.
Escape the Vape Video Challenge Returns for 2023
The Escape the Vape Video Challenge, a youth vaping prevention video contest, is back for 2023. Minnesota middle and high school students are invited to create and submit a 30-second public service announcement (PSA) video to educate their peers on the dangers of e-cigarette use, also known as vaping. Submissions will be entered into a competition for cash prizes for both students and their schools.
Key Contest Dates
- February 1, 2023 – Video Submission Opens
Students will have the month of February to finalize and submit their videos - February 28, 2023 – Video Submission Deadline
- March 24, 2023 – Finalists Announced
- March 24 - April 6, 2023 – Public Voting
- April 7, 2023 – Winners Announced
Minnesota Youth can learn more about the Escape the Vape Video Challenge and submit their video at mnescapethevape.org.
For more information on sponsorships or how to promote the contest with youth in your community visit Escape the Vape Video Challenge.
New Data Brief: SHIP supports local Tobacco 21 policies, helping to reduce youth commercial tobacco use
National data indicate that about 90% of adults who smoke start before age 18, and 99% start before age 26. Statewide Health Improvement Partnership (SHIP) partners across the state have worked to support the implementation of local Tobacco 21 (T21) policies that raise the tobacco purchase age from 18 to 21. Between July 2017 and January 2019, 17 Minnesota communities implemented a T21 policy, and 14 of these received SHIP support. By December 2019, 60 Minnesota communities had implemented local T21 policies prior to the federal version of the law taking effect.
Data from the Minnesota Student Survey (MSS) indicate that these policies have been successful at reducing youth commercial tobacco use. Minnesota 8th and 9th graders who were protected by T21 policies reported less commercial tobacco use than those living in communities without T21 policies.
Read more: SHIP supports local Tobacco 21 policies, helping to reduce youth commercial tobacco use
Minnesota has made historic progress
Thanks to effective, evidence-based policies that ensure clean indoor air and keep commercial tobacco prices high, Minnesota’s smoking rates are the lowest ever recorded.
Among 11th graders, smoking fell from 12.2 percent in 2013 to 8.4 percent in 2016. Among adults, smoking fell from 16.1 percent in 2010 to 14.4 percent in 2014.
Learn more about youth commercial tobacco use.
We have more work to do
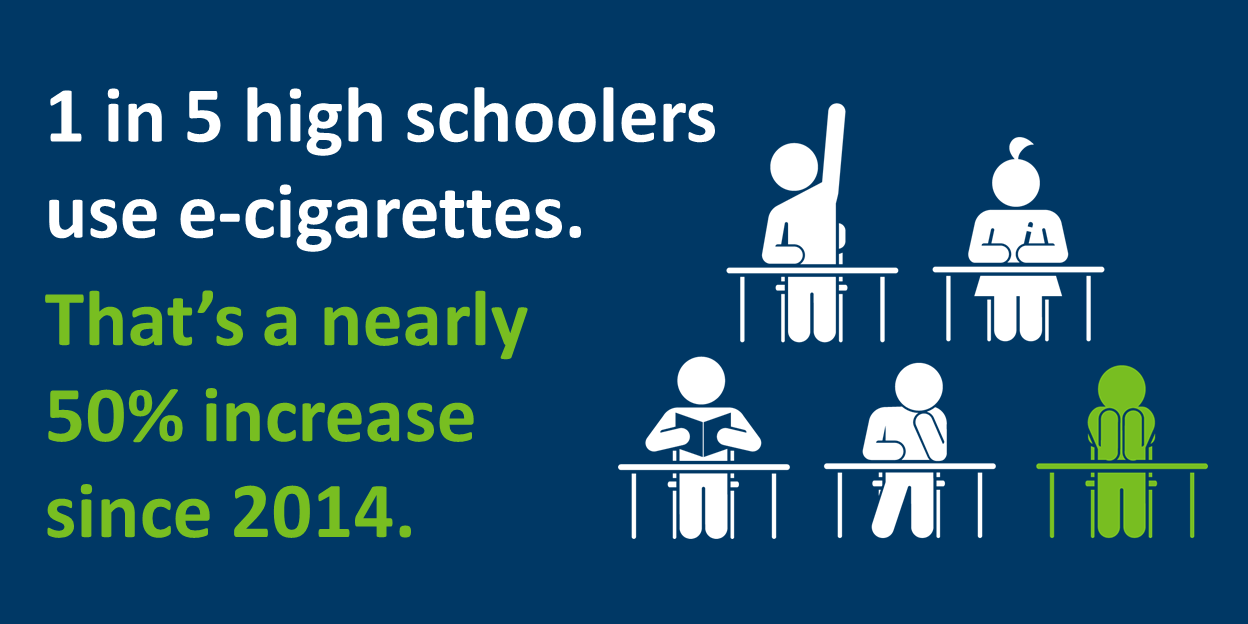 More kids are using new and flavored products, like e-cigarettes. E-cigarette use is twice as high as conventional cigarettes. Nicotine, found in these products, is highly addictive and harmful to the adolescent brain.
More kids are using new and flavored products, like e-cigarettes. E-cigarette use is twice as high as conventional cigarettes. Nicotine, found in these products, is highly addictive and harmful to the adolescent brain.
Learn more about e-cigarettes and other vaping products.
Many communities also still use commercial tobacco at significantly higher rates. Culturally appropriate and community-led efforts are needed to close these gaps.
Trying to Quit Smoking, Vaping, or Chewing?
 Quit Partner is Minnesota’s family of programs to help people who want to quit smoking, vaping, chewing, or using other commercial tobacco products. Call 1-800-QUIT-NOW (784-8669) or visit Quit Partner.
Quit Partner is Minnesota’s family of programs to help people who want to quit smoking, vaping, chewing, or using other commercial tobacco products. Call 1-800-QUIT-NOW (784-8669) or visit Quit Partner.
For more help, visit Quitting Commercial Tobacco.