Minnesota Health Equity Networks Newsletters
To find these monthly updates directly in your inbox, subscribe to the Minnesota Health Equity Networks newsletter.
May 2025
Mission and Momentum: Spotlight on Goodhue County Health and Human Services

Numerous committees, subcommittees, and teams have all contributed to the health equity efforts in Goodhue County, and the work is ongoing. Kris Johnson is the Deputy Director of the Goodhue County Health and Human Services (HHS) Department, and since 2020, has co-facilitated the County Equity Committee as well as the HHS Equity Committee. She brings a wealth of experience and history to equity work in the region. Kris is a strong advocate of community engagement and believes that it is critical to success in health equity work.
“The term 'equity' is so often misunderstood, which can get in the way of doing the work. In public health, we need to understand our community and recognize that we can’t have a one-size-fits-all solution for every issue.” - Kris Johnson, Deputy Director, Goodhue County HHS
The Goodhue County HHS Equity Committee was first established in 2016. In June 2020, following encouragement from County Commissioner Anderson, a countywide equity committee was formed to expand the efforts across all county departments. By September 2020, the Goodhue County Equity Review Team became a standing committee of the County Board.
In April 2021, consultants from AMAZEworks were brought in using COVID funding to guide the group and build capacity. In partnership with AMAZEworks, committee members and leadership completed the Intercultural Development Inventory to evaluate their strengths and growth opportunities. Through this process, they learned that most county staff had limited experience with people of different cultural backgrounds, and efforts were made to increase exposure to multiple cultures.
“We now have ongoing internal trainings on equity topics with required attendance. Employees are also allowed up to six hours paid time per year to attend cultural events like powwows or Hispanic heritage celebrations. Beyond this, we provide training on bias and belonging to all county departments.” - Kris Johnson
The HHS Health Equity Committee also works on building a more inclusive and equitable departmental environment. A Customer Input Subcommittee was formed to help guide those efforts and it launched a Customer Satisfaction Survey, piloting a system to collect feedback and improve services and access.
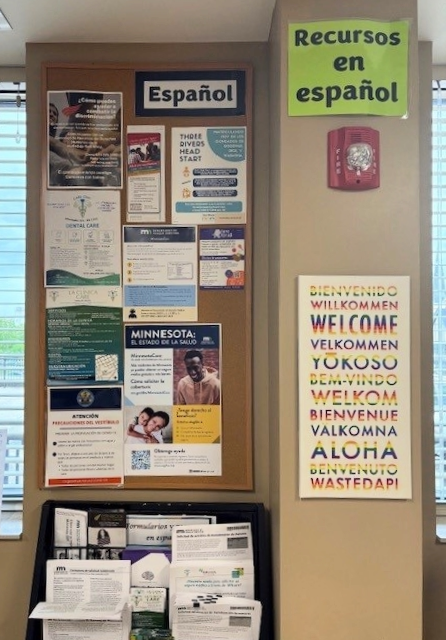 Anna Kohlnhofer, community health specialist, assists the ongoing efforts of the Limited English Proficiency (LEP) Liaison Subcommittee. This subcommittee supports a number of impactful projects, including community outreach, evaluation of personnel policies, and departmental collaboration.
Anna Kohlnhofer, community health specialist, assists the ongoing efforts of the Limited English Proficiency (LEP) Liaison Subcommittee. This subcommittee supports a number of impactful projects, including community outreach, evaluation of personnel policies, and departmental collaboration.
“We don’t want to just check boxes but develop effective dialogue and approach our work in a meaningful way. We also share training and resources with other county departments and work to eliminate silos.” – Anna Kohlnhofer, community health specialist, Goodhue County HHS
In addition, a cultural liaison now helps with interpretation and translation and brings an additional equity lens to client services. Spanish language sessions are provided for staff, and HHS continues to offer other cultural and language learning opportunities on an ongoing basis.
The Goodhue County Equity Committee recently changed its name and now is called the Goodhue County Engagement Committee. Kris explained, “We decided to “rebrand” our committee to emphasize the need for engagement—both internal engagement with our staff and external engagement with the communities we serve.” Despite the name change, Anna says other, more important things stay the same. “Our mission, vision, and values haven’t changed. And we’re not going to stop this work.”
Each equity committee, subcommittee and team in Goodhue County has formed their own unique identity, timeline, and approach, but all of them have the same goal: to forward health equity and positively impact the residents of their county.
“These steps have built momentum toward a more equitable and welcoming environment for everyone in Goodhue County. That’s what public health work is all about.” - Kris Johnson
Goodbye, for now
Message from Shor, project supervisor

Hello, networks communities,
As the heat and activity of summer approaches, I hope you are finding joy in anticipating the lakes, fireflies, bonfires, swimming, gardens, flowers, ice cream, and whatever else brings you a smile in this season. Personally, I am looking forward to picking some juicy strawberries.
Along with those juicy strawberries, I will also be starting a juicy new job in June and will be bidding my Minnesota Health Equity Networks team and all of you a bittersweet goodbye. It truly is sad for me to step away from this team that I have been working with for three years and have grown to admire and love. I appreciate our collaborative and soulful work together and will deeply miss working with each of our partners as well. I will particularly miss supporting the work of advancing health equity across the state by nurturing and growing relationships in so many ways. It has been a dream to be a part of this work and this team.
My next adventure will not be taking me far away, as I will continue to do equity work from a slightly different angle by managing the City of Minneapolis LGBTQIA+ Programs. I am thrilled to focus on this work and to support the City of Minneapolis in its ongoing commitment to our LGBTQIA+ communities.
While this is goodbye for now, I know that this work is in the best of hands, and I can't wait to see it continue.
With much pride and joy,
shor
The Corner: Farewell messages from the team
Reflections and farewell messages from the Health Equity Networks Team as Supervisor Shor Salkas prepares for their next adventure.

“Shor, I’ve deeply admired your leadership and learned so much from the way you’ve guided this team with care and compassion over the past three years. Thank you for fostering a healthy, supportive environment where we could all thrive in our work.” – Fa Youb, Central Regional Health Equity Network coordinator
“Shor provided both a vision and a platform for the work of the networks and for the formation and progress of our team. They demonstrated how to enhance and maintain genuine connection in all parts of work and life and encouraged us to cultivate our own relationships, strengths, and skills. As Shor moves into a new role, we can only say thank you and try to do them proud.” - Colleen McKinney, Northeast Regional Health Equity Network coordinator
“Shor has been a true leader with integrity, respect, and kindness. They have held space for us to heal, learn, and have honored our humanity as we have built the networks together. I look forward to continuing to partner with Shor and learn from them as they continue to make an impact on equity in Minnesota. Shor, your heart and story will continue here in our work and your energy and passion will be missed.” – Lyndsey Reece, Southeast Regional Health Equity Network coordinator
“I could not have written a better role for Shor to shine in as their new position leading the LGBTQ inclusion work with the City of Minneapolis, but I am sad about not having Shor as our fearless leader for the Minnesota Health Equity Networks. I am in deep gratitude for Shor's work in creating a clear north star to guide how we show up as a network and what values drive our work. This is a house you built, Shor, and it has a strong foundation!” - TC Duong, Health Equity capacity building specialist
“Shor's dedication to equity shines in all that they touch. Shor consistently fosters a sense of inclusion and provides a level of support that enables our team to thrive. Their lasting impact is baked into the work we do. I couldn't be more excited for what Shor's next opportunity will entail, and all the lives they will touch in that work!” – Ben Cahill, Northwest Regional Health Equity Network coordinator
Past Minnesota Health Equity Networks Newsletters
2025
Spotlight on 100 Rural Women: Creating connections and inspiring leadership
Teresa Kittridge says her life story has often been shaped by a “gap in leadership,” created by the fact that women are significantly underrepresented in formal decision-making roles in rural America.
“Women are leading every day in (rural) communities. They just are not in formal leadership roles and that’s what we’re trying to see more of. I think that a solution to cut through the political divisiveness in rural (areas) is to have more women leading.” - Teresa Kittridge, Founder and President, 100 Rural Women
The nonprofit, nonpartisan group 100 Rural Women got its jump-start in 2019 when Teresa invited a handful of women to join her in Marcell, Minn. They spent the day focused on needs, assets, and how to better support each other. Every woman in that room raised their hand to help make 100 Rural Women happen.
Our initial research was from 100 meetings we held across the state of Minnesota. All of our programming emanated from that research.” – Teresa Kittridge
The organization sees young women’s leadership as key to the future of rural life. From the beginning, having at least 50% of its board members under the age of 30 has been a priority. Teresa says this effort fit in with a central theme in their programming, which is mentorship. She told us, “I encourage our young women to follow their passion, and I love to watch where they are going. We practice circular mentorship. We mentor them, and they mentor us.”
For example, when COVID-19 brought significant challenges, the younger women on the team helped the organization successfully navigate the pandemic by bringing a virtual approach that continues today. Teresa says it has widened the scope of their efforts to include more national and international connections.
“[COVID-19] pushed us to adapt quickly, get creative, and find new ways to deliver programming, conduct research, and provide support. We’ve had more reach. It’s not perfect, but it removes barriers for women who are balancing so much.” - Teresa Kittridge
Challenges have been and continue to be a concern. Funding is always an issue for small nonprofits. The organization is fortunate to have a few funders who understand the women’s leadership crisis in rural areas. These funders, along with pro bono services and private donations, created a culture of support and have kept 100 Rural Women operating through many financial ups and downs. Nonetheless, Teresa is surprised at how difficult the process has been.
“I am continually astounded by the lack of understanding—and often, interest—among funders regarding the equity gap and the underrepresentation of women in formal leadership roles in rural areas.” – Teresa Kittridge
She says another of the most crucial hurdles to overcome has been working to “build a nonpartisan and non-issue-oriented organization during a time of intense polarization.” With characteristic positivity, Teresa adds, “it has shaped our resilience and focus.”
“I look for those pieces that people can work on together. I work to find two or three things we agree on. People need to feel safe and discuss what’s important to them.” – Teresa Kittridge
In its five years of operation, 100 Rural Women has worked with over 50 interns and graduate students, established multiple partnerships, launched a mailing list of over 5,500 subscribers, and developed innovative and successful programming. Teresa says that she recognizes the importance of continually infusing fresh vision, next-generation leadership, and new energy into the work. Because of this, the year 2025 is focused on evaluation, engagement, visioning, leadership, and sustainability. In May, they are launching a new podcast featuring the stories of 100 rural women. And each day, 100 Rural Women will continue to lead for positive change.
“I’m excited to collaborate….to identify opportunities that will propel our work into the future. It has truly been an honor to be part of this meaningful journey.” – Teresa Kittridge
A bittersweet spring
Message from Shor, project supervisor
Hello networks partners and communities,
We write to you a little later than anticipated as we have been navigating a great deal of change and turmoil at the Minnesota Department of Health (MDH). As I am sure many of you have seen and experienced the impact of, a few weeks ago MDH received notice of a massive funding cut from the federal government which led to dozens of grants and contracts being terminated and hundreds of employees and contractors receiving layoff notices.
This has been an incredibly difficult and chaotic moment for us and our partners across the state, and we are so sorry that we have all had to experience this change in this way. And…as we continue onward toward the return of warmer weather, budding plants, and the sweetness of spring, I, again, encourage you to pause to let the sweetness wash over you whenever possible. It is one way to practice self-care in a time of rapid change.
We have been hearing from you that things are challenging and confusing in many ways. Knowing what to do and how to take care of yourself and others can feel pretty hard. We want to honor the moments we are all living through by offering some new opportunities in response to your feedback. We invite you to attend:
- The Networks Open Space Gatherings, which will be scheduled every other month. This space is for people to join as needed to discuss or troubleshoot what is emerging in their communities, workplaces, and in the public health system. You will network with our coordinators, staff members, and other community members. We will strive to create a space that is welcoming, supportive, friendly, and as confidential as possible. In March, our first Open Space was well-received by folks from across the state.
- The Networks Restorative Practice Gatherings, which will be a series of 30-minute sessions offered in April and June where we offer space to pause and work toward lowering stress and anxiety. Through experiential learning sessions, participants will gain experience with techniques and exercises that can bring restorative practices into their work and life.
- The Networks Coaching Pilot Program, which offers the opportunity to work either one-to-one or in a small group with a coach to get support on issues you are working through! Coaching can be a great space to explore or troubleshoot workplace, equity, or engagement issues or any others you may be dealing with, all with the advantage of a coach in your corner. If you are interested in learning more, reach out to Lyndsey (lyndsey.reece@state.mn.us). There is limited space in this initial pilot program.
We look forward to continuing to be responsive to the ever-changing needs of our communities as we move forward in this time of both spring sweetness and rapid change.
Much care to you,
shor
The Corner: Technical assistance with TC
Reflections and activity highlights from Capacity Building Specialist TC Duong.
Technical assistance and capacity building is not just my job but also my joy. I get a front-row seat by working to fulfill training and technical assistance requests. It’s always gratifying to see how partners in our networks have grown in understanding the many ways that health equity lives in their work.
“Technical assistance” can sometimes be a vague term, so I want to take this opportunity to share a few details about the support that we offer.
- Training - Trainings are topic-specific sessions designed in increase knowledge and understanding of the frameworks, practices, and mindsets of health equity. We offer trainings around topics like: Foundations of Health Equity, Community Engagement Basics, Implicit Bias and Cultural Humility, Ways to Talk About Health Equity, and Intersectionality and Equity.
- Facilitation - Our facilitation efforts are designed to create conversations and processes with your team that move you toward your equity goals. This might include preparing for an equity analysis, developing a community engagement plan, or applying an equity lens to a policy or procedure.
- Resource Support - Network coordinators and other staff work with partners to connect with others in their region, with MDH staff, as well as with other community resources (including introductions to community organizations, lists of consultants, online resources, and readings and case studies) depending upon the specific request.
We welcome requests for technical assistance and value the wisdom of the partners who work to promote health equity in our Minnesota communities. Our goal is to make sure that the content we provide meets your needs and reflects your unique perspectives.
The first step is to complete a short form: Minnesota Health Equity Networks - Training, TA, and Facilitation Request Form. Once that is done, a health equity team member will connect with you and set up time to talk about the request.
Please feel free to reach out to me at any time if you have questions or need further information. I look forward to connecting with all of you. After all, it is my job and also my joy to provide these services to our partners!
-TC Duong, Health Equity Capacity Building Specialist
Spotlight on: The Center for Victims of Torture, St. Cloud
Mental health issues and topics are always challenging. But for victims of trauma and torture who are new to the United States and whose cultural traditions may view mental health differently, the complexity of addressing these issues expands significantly. The Center for Victims of Torture in St. Cloud has faced these challenges for decades, and their team has learned to adjust and provide needed support to the community in ways that respect and acknowledge their cultures and experiences.
According to the center's website, there are more than 50,000 torture survivors living in Minnesota. They are adults and children who have endured devastating events and are now rebuilding their lives in a new community. Many hear about the center through outreach and education sessions within their communities. Some find the center through word of mouth as well as referrals from health care and legal and community services organizations.
One of the many initiatives at the St. Cloud center is a series of parenting classes, which teaches methods of working with children who assimilate to the new language and environment more rapidly than adults. Started in 2017 as part of community education offerings in area school district, the classes help families manage new situations.
“Everyone was a parent to every child in Somalia, but here it’s different. Many parents think they don’t have rights in America, so it’s very important to teach them how the system works in the United States. They don’t know their role here.” – Mathar Abdullahi – bilingual community educator and case manager, Center for Victims of Torture
The team in St. Cloud also developed programs to share information about mental health care and support and then integrated these topics into the parenting curriculum. This approach offers an opportunity for community members to learn about complicated and complex issues in a less threatening environment.
“Some of these topics are hard to talk about. It’s scary for people to talk about mental health stigma, and it’s hard to talk about the trauma and torture they experienced. This way we can provide learning opportunities and raise community awareness.” – Hanan Barud, bilingual community educator, Center for Victims of Torture
When COVID arrived, radio played a key role in the community. The center worked to help people understand the risks and how to prevent the spread of the virus by broadcasting translated information. Announcements and updates from the city of St. Cloud, the school district, the police department, and other organizations were also translated and broadcast on the Somali community station St. Cloud Somali Community Radio. The team broadcasted other topics of benefit to the community, including the curriculum used for parenting classes. Established community members were brought in to talk about community issues and provided even more trusted sources of information.
The center also conducted parenting courses virtually and provided training to community members on how to access the classes via tablets and cellphones. This virtual option was very well received and is still offered.
The center continues to make progress in achieving its mission. In 2022, case management and psychotherapy providers with lived experience with the cultural backgrounds of those seeking services joined them. Additional center broadcasts are now aired on St. Cloud State University campus radio. This year, a women’s support group started. And above all, community members are now more open to getting mental health assistance and intervention. But there is always more to do.
“The programs are funded from many sources, including grants and donations. We’d love to expand our services, but funding constraints are always an issue.” – Abdigani Ahmed, program manager and psychotherapist, Center for Victims of Torture
The center continues to face challenges. Staffing frequently shifts between part-time and full-time in response to budget changes, and an international organization like the center faces added layers of complexity. Despite this, the team at the St. Cloud center relies on creativity, communication, and a shared culture to navigate these challenges.
Finding hope and energy in change
Message from Shor, project supervisor
Hello networks partners and communities,
As we head into spring and we (literally) thaw out, we are also stepping into a whole new way of being in the world. Spring often brings mud as well as buds and can also offer exciting new energy and hope. I invite you to try to stay in that positive energy as much as you can in this work, especially if or when it starts to feel different, hard, and devalued.
The work of health equity has never been more important, but we need to approach it a bit differently right now. One approach is to think outside of the phrases and words about health equity that we are accustomed to hearing or reading. Instead, ask questions that help us consider the ways that we are doing this work. Examples of questions to ask are:
- When I think about the people and communities I serve, how do I know that I am truly serving everyone?
- Who might be left out and why?
- What are my sources of information?
- How do I broaden what I know?
- When I consider how I do my work, am I considering the people and communities I serve while in the process of planning and creating possible solutions?
- When I consider how I do my work, am I taking into consideration whether it is accessible and the communities and people who want to participate have what they need to do so?
These are just a few questions to consider. There are many other ways to talk about, think about, and do this work. We at the Health Equity Networks are here to help and support you in that.
As part of that help and support, we will begin hosting a series of Networks Open Space sessions in March. There will be no agenda during these sessions, but simply an opportunity for our partners across the state to discuss and troubleshoot what is emerging in their communities, workplaces, and in the public health system. We will strive to create a space that is welcoming, supportive, friendly, and as confidential as possible.
Join with network coordinators, staff members, and other community members at our first Open Space session at noon on March 18. Bring your lunch!
Spring mud brings challenges to all of us, but spring buds will arrive. I trust that they will offer us new energy and hope.
Take care,
shor
Coordinator's corner: Host a mini gathering and share your expertise!
Reflections and activity highlights from the regional coordinators.
To further connect network partners, our team offers mini gatherings as an opportunity to focus on specific topics, highlight partner accomplishments, and, above all, learn from each other. They are a powerful way to bring together individuals who have a working knowledge and expertise in topics that can benefit all of us.
For example, in a recent mini gathering, we heard from Project Reach cohort member Dan Wilson, who presented information on well water and its impact on health in Southeast Minnesota. This mini gathering brought together others who shared their awareness of the well water situation in Minnesota and offered some possible solutions. Because we learned from each other and made connections, this mini gathering had real impact. Since then, many network members are planning to work to raise awareness of the well water issue and build on the positive energy created.
We at the networks hope to continue to cohost more mini gatherings in the future. We believe that you are the experts on important and relevant health equity topics and efforts, and we invite you to share your expertise. Please reach out to your regional coordinator if you are interested in cohosting and leading a mini gathering. Topics could be anything that you find important to wellness in your communities.
This is a callout to you, our network partners! Through our regional and statewide gatherings, one-to-one conversations, and spotlights, we have learned much from you. We look forward to learning even more.
Lyndsey Reece, Southeast Minnesota Health Equity Network coordinator
Spotlight on: Le Sueur and Waseca Counties
In Le Sueur and Waseca Counties, a dedicated team of public health professionals serves their communities with equity at the forefront while leveraging data to meet future goals. Above all, their own lived experiences, as well as those of their family members, give them insights into community concerns and help to establish meaningful relationships and connections.
Colin Ayers is the community health educator and planner for Le Sueur and Waseca Counties. When he started the position three years ago, he focused on data collection and analysis. Now, he’s also the project lead in areas like mental health, cannabis, opioids, and communications.
“What inspires me to go to work every day is knowing that I have an opportunity to give back to the community where I was born and raised.” – Colin Ayers
In 2021, Mariana Izaguirre became the first certified community health worker in Waseca County. Through a state grant, she earned a certificate from St. Catherine’s University, and now uses her skills and background to assist in cultural awareness, communications, and translation throughout the public health departments.
“People who only speak Spanish feel like they’re being a bother. We are changing this by building relationships. I like to say I’m a piece of all our services.” -- Mariana Izaguirre

Le Sueur and Waseca County staff participate in a community tabling event.
Trisha Chimal-Simonette is an administrative assistant at the public health office in Le Sueur County, but her role goes well past any job description. She speaks Spanish and is involved with the community, so she gets visits and calls almost daily from folks looking for assistance. She says she always tries to listen and identify the real issues and root causes.
“My family has personal stories that have affected our lives forever and taught me much. I live and breathe health equity daily because of my own family dynamics. I wear my public health hat, but it’s also about being a human being.” -- Trisha Chimal-Simonette
Colin, Mariana, and Trisha play numerous roles within the county’s public health. Their collaboration and contributions have resulted in new projects, including:
- Power of Produce (PoP) Club: The PoP Club helps children aged 0 to 18 get access to fresh produce. This collaboration is with the Statewide Health Improvement Partnership (SHIP), County 4-H, Master Gardeners, and the Waseca Library. In 2023, 587 kids from 33 different communities participated, and in 2024, $5,896 was spent at the farmers market with 32 vendors participating.
- Mental Health Awareness Project: This activity began with a project Colin organized with SHIP collaboration, which aimed to destigmatize mental health, encourage conversations about mental health, and provide mental health resources. The project promoted the passing of a mental health proclamation and started a suicide cohort.
- Rock Painting and Rock Garden Mental Health Project: A part of the Mental Health Awareness project, this included a rock painting event at the Waseca Public Library as well as the distribution of rock painting kits to daycare centers in Waseca and Le Sueur Counties. Mariana took the project further and created a community rock garden that addresses mental health issues through art.
- All About Newborns: This project will start in March 2025 in collaboration with public health nurses. All newborn caregivers will have access to a nurse, baby weight checks, breastfeeding support, and education on various newborn topics in a group setting. No income guidelines or other qualifications are needed to attend.
Colin said that these projects began by completing the community health assessment and community health improvement plan (CHA/CHIP) and analyzing the data that they revealed. He also learned the value of creating information that is easy to understand, worded clearly, and readable. Trisha added, “We need to keep it simple.” Mariana said it is important to think about cultural differences, perceptions, and interpretations and clarify understanding. And, above all, to maintain relationships.
“I learned that having a relationship with our community members is essential to getting messages across. Having events open to everyone surprised some people, but it was a great idea!” -- Mariana Izaguirre
There are many challenges to their efforts, and Colin constantly works to find new ways to collect and communicate data. He said he thinks it’s important to back up what they do with data and to use that data to gain funding.
“Our work furthers health equity because it helps identify gaps in the health of our communities. Plus, it also gives us a chance to develop deeper, more impactful relationships with the communities we serve. We can better understand what is needed to make sure everyone in our community has access to the healthiest life possible. Yes, we’re rural, yes, we’re small, but we’re trying it out.” – Colin Ayers
New year, new hires, and a new division!
Message from Shor, project supervisor
Our team is excited and eager to welcome 2025. This year is bringing many changes to the Health Equity Networks, and I am taking the opportunity to share the details with you here.
We have a new Northwest Regional Health Equity Coordinator! We are thrilled to welcome Ben Cahill. Ben is picking up the baton from Mary Mitchell and is already a valuable team member. He introduces himself in this newsletter’s Coordinator’s Corner below, so please read it and get to know him.
We are also in the process of hiring a new Southwest Regional Health Equity Network Coordinator. More information will be available soon as we move forward with the hiring process.
Our other big change is that our team has moved to a new division within the Minnesota Department of Health. As of Jan. 15, we joined the Health Equity Strategy and Innovation Division. We are thrilled to be part of a cohort of colleagues who are deeply committed to advancing health equity in so many different ways and in so many different communities. We are also excited to collaborate further with our new colleagues on community engagement, systems change, and other health equity practices. In the future, we hope to bring more information on these collaborations to our partners and communities through the Networks’ gatherings and trainings.
We are still learning our way in this new place. We appreciate your patience as the dust settles!
Take care, and see you soon,
shor
Coordinator's corner: Meet Ben!
Reflections and activity highlights from the regional coordinators.
I’m Ben, the new Northwest Regional Health Equity Networks Coordinator, a Seattle-area transplant who moved to in Bemidji in 2020. In 2021, while working at Sanford Health, I earned a Community Health Worker certificate at Northwest Technical College. I then went on to work for PrimeWest Health and the Red Lake Nation. I enjoyed assisting individuals in navigating health care and social service systems, getting connected with resources, and advocating alongside of them. I also participated in the 2023–24 U of M Cohort called Project R.E.A.C.H., which focuses on empowering those in community and public health to make a difference through legislative advocacy and public policy.
While doing this work, I learned a lot about health disparities and social determinants of health. I can’t wait to use that knowledge and experience in my work with the Health Equity Networks!
I’m currently studying social work at Bemidji State University. Additionally, as an Initiators Fellow with the Initiative Foundation, I am working to create a non-profit organization designed to empower and connect LGBTQ2S+ individuals in my area. I enjoy cooking, sharing a laugh with friends, and hosting a local LGBTQ2S+ karaoke night, “Queeraoke.” It has been a joy to have a safe and expressive place here in the Northwoods.
I am excited by the opportunity to fill the role of Northwest Regional Coordinator and strengthen, amplify, and connect the health equity work in the region and the amazing people behind it!
Reach out any time. I look forward to doing this important work with you.
Warmly,
Ben Cahill
2024
Spotlight on: Dancing Sky Area Agency on Aging
Named for Minnesota's northernmost scenic drive, which travels along the Rainy River from Voyageurs National Park near the Canadian border west to North Dakota, the Dancing Sky Area Agency on Aging supports a 21-county area. Like the scenic drive it’s named for, Dancing Sky covers a vast area of mostly rural communities. Because of this, it encounters both challenges and opportunities.
Dancing Sky is a program of the Northwest Regional Development Commission and collaborates with many partners and providers. They coordinate the pass-through funding intended to enrich the lives of older adults and their caregivers and operate the highly rated Senior LinkAge Line services.
“We play a unique role in our communities. We want older adults to thrive. That differs from community to community. Above all, we work to fill service gaps and focus on the needs of those we serve. The Older Americans Act, along with the Senior Linkage Line, is the core of what we do.” - Heather Pender, Dancing Sky director
Heather Pender has worked for Dancing Sky for ten years and is now entering her third year as director. She is proud of their collaborative work and successes and calls Dancing Sky “the best-kept secret" in the region.

The Older Americans Act funds various services designed to help older persons secure and maintain independence and dignity in a home environment, remove barriers for older persons, and provide a continuum of care for older and vulnerable adults. Additional services support family, friends, and neighbors who care for older persons, grandparents, and older relatives who care for children. Service options includes community classes, educational presentations, caregiver resources, support groups, respite care, congregate nutrition, and home-delivered meals.
The Senior LinkAge Line offers information, connects people to services, and provides help making informed personalized decisions. Phone specialists are also certified health insurance counselors who can assist with Medicare. In addition, Resource Coordinators help with in-depth person-centered planning for consumers and caregivers. They are focused on keeping people in their homes or returning them home from a care facility.
Above all, Heather says, there is “no wrong door” when people contact Dancing Sky. "We connect them to where they need to be, even if it’s not us.”
“In rural Minnesota, our needs don't differ from those in the more urban areas, but living in a rural area does impact the ways we respond. There are fewer opportunities in rural areas, so we have learned to leverage what we have.” -- Heather Pender
Dancing Sky identifies possible partners by finding providers or organizations that can expand their services. Heather says that partners “wear so many hats, do so many things,” sometimes funds may need to be spread out over several providers, or providers may need to consider ways to implement grant funds successfully.
“It’s all about starting small and gaining. We are lucky to partner with providers who share the same mission, vision, goals, and view of health equity that we have.” - Heather Pender
Heather says that rural Minnesota communities are at a crucial point. Life in rural communities brings numerous challenges for older adults, such as limited access to services and supports, nursing home closures, and barriers to transportation, particularly for medical and accessible transportation. Shrinking service budgets don’t meet community needs, especially those used to fund senior meals.
“There is an urgent need for planning and services as more people age. We must advocate for funding for a rapidly growing senior population. Covid services helped to showcase this, but we need other funds. Now is not the time to rest when advocating for older adults.” – Heather Pender
This year, Dancing Sky received American Rescue Plan funding, and they have launched a pilot program in partnership with other Area Agencies on Aging and the Minnesota Department of Human Services. The program will use the funds to reduce the risk of maltreatment of vulnerable adults. Referrals for services and support come directly from the counties.
In 2024, the Agency also provided technical assistance to communities to become more age-friendly and helped them focus on grants that can support that work. The Agency development team offers monthly webinars and a variety of trainings that promote Age-Friendly Minnesota status throughout the region.
Heather credits the success of Dancing Sky to the efforts of staff and partners. In 2025, she hopes to continue the advocacy work, secure more funds for senior nutrition, and maintain the adult protection pilot project.
“Everyone has a story related to aging. We are all here for a reason that's bigger than a paycheck. As an agency, we do our best to partner with providers doing great work, filling gaps, and meeting needs. It's a good feeling knowing that we are making a difference in someone's life." - Heather Pender
Navigate the holiday season with care and connection
Message from Shor, project supervisor
As we head into the darkest days of the year, we welcome you to remember that we can invite rest even in these moments of darkness. Our culture doesn't often support us in prioritizing rest, and we all need it sometimes.
During this season of darkness, I also invite you to light a candle if you can (rather than turning on a light) and look in a mirror using just the candlelight. And ask yourself, "What seems different?" The answer might be truly enlightening.
As we move through this time of the year, our team has undergone several staff transitions and other changes within the Minnesota Department of Health (MDH). At the end of December, we will be saying farewell to our Northwest Regional Coordinator, Mary Mitchell, as she moves on to new adventures in her life. I am grateful for the care Mary brought to her role in the Northwest region. She truly demonstrated how to build relationships grounded in curiosity and kindness, and then she supported the growth of those relationships and networks across the region. Our next Northwest Coordinator is already set for success due to Mary's amazing work! We will announce the name of our new Northwest Coordinator in the January 2025 newsletter.
Our team is also undergoing a transition within MDH. Over the last few years, we have grown this work from within the Community Health Division. In the New Year, we will move to the Health Equity Strategy and Innovation Division within the Health Equity Bureau. We are excited about working more closely with our beloved colleagues in this division and looking forward to creating strong alignment and programming with them. Any move comes with a lot of learning, and that is what we are currently doing. We hope you won't mind the dust as we settle into a new space!
Over this holiday season, please take care of yourself in ways that are meaningful to you, your family, and your culture.
More to come in the new year,
shor
Coordinator's corner: Farewell from Mary
Reflections and activity highlights from the regional coordinators.
As I bid farewell to MDH and the Health Equity Networks at the end of December, I have been reflecting on the work my team and I have done over the past three years. So many memories and emotions are surfacing that I have been getting a little sentimental.
When I accepted the Health Equity Network Coordinator position in 2021, I had no idea what a life-changing experience it would be. I was interested in this work because I am passionate about improving the health outcomes for all people in my community and region. I recently retired as the director of a regional food shelf and thought this project would be perfect for my work and life timeline.
I am incredibly proud to have been a part of creating the Health Equity Networks with my thoughtful and creative team members and our regional partners. We have all grown and learned together since taking our first wobbly steps back in 2022. Now we are dancing.
My favorite part of the work has been the many one-to-one meetings with my region's partners. I especially value the opportunities I had to visit leaders where they live and work. I learned so much about the critical services they provide to their communities and how they strive to advance health equity.
The dance continues with some new faces, opportunities, and challenges. I am excited to see what the future holds for the Networks and this work. I am grateful to everyone who has walked and danced alongside me in the past three years.
With gratitude,
Mary Mitchell, NW Regional Health Equity Network coordinator (outgoing)
Spotlight on: Human Libraries, Bemidji State University Social Work Department’s Immersive Learning Experience
The Human Library at the Bemidji State University (BSU) Social Work Department gives a whole new meaning to the phrase "I'm an open book." After Assistant Professor Emily Paine learned about the Human Library Experience, she introduced this innovative concept to the department in 2022. Since then, it has been an integral part of the curriculum in two courses. Assistant Professor Ashley Charwood describes the Human Library as a "microcosm" of the real-world experiences students will encounter in their social work practice.
"Instead of checking out a book, you have a conversation with a person. We are all walking and talking stories." – Emily Paine, Assistant Professor, Bemidji State University Social Work program
According to the Human Library website, it is "a place where difficult questions are expected, appreciated, and answered." Stereotypes can be challenged by hearing stories directly from real people and asking questions about their life experiences. As a result, people can be better understood.
Ashley explains that integrating the Human Library experience into social work classes offers a unique opportunity for preparation. Students craft and practice their questions, considering factors such as nonverbal communication and environment. After the "readings," students reflect on their experiences. Emily refers to this lead-up and follow-up process as "bookends." "These human book experiences challenge their biases and assumptions," she says. "They prompt students to ask themselves, 'Why did I think that?'"
“This experience allowed me to see different experiences through the eyes of the beholder...to understand that what is really important is the person who is speaking and how they feel…I believe that this taught me to learn while I listen...” - BSU Human Book Student
Human books are personally recruited and referred by students and community members, or sometimes they volunteer. If they agree to participate, a “book description” is created for each of them. They are in contact with the Social Work Department staff, who provide examples of other book descriptions and offer assistance in writing their own or creating their "book.”
Human book participants are encouraged to reflect on the power of sharing their story, ensuring they understand what to expect. Additionally, time is built into the event for human books to answer questions if they choose to do so.
"Storytellers are taken care of. This process is not done in a voyeuristic way, and everyone involved is met with compassion. We nurture the books and the humans.” – Emily Paine
Human books may tell their stories up to three times at an event, and the narrative sometimes changes as they do. Many find the experience to be empowering and return for another session.
“Thank you for the opportunity! It’s been healing to share with everyone today. I feel supported and uplifted. Chi Miigwech!” - Human Book Storyteller
Students are given a list of book titles to choose from before the event but have the opportunity to change their plans on the spot. Emily says, “The power of this is that it's a dialogue. All involved must show up and bring their best selves to be present. It builds on small groups, and then it becomes the 'magic of the moment.'"
“With the Human Library, the gift is given both ways.” – Ashley Charwood
To learn more about Bemidji State University's on-campus and online Social Work Program, visit their website: Social Work | Bemidji State University
Here are some of the resources about the Human Library:
- Unjudge someone - The Human Library Organization
- Human Library Explained in a Minute
- "Unjudge Someone,"- A short film about the Human Library.
Here are some readings about the benefits of sharing your story:
- The power of storytelling to facilitate human connection and learning
- The power of your story
- Transformative power of storytelling
Navigate the holiday season with care and connection
Message from Shor, Project Supervisor
As we roll into the holiday season, we at the Networks wish you joy, warmth, and connectedness.
This time of year can bring us much delight. It can also bring up issues related to family dynamics, safety, and historical trauma. For many, the feelings are of pain and grief. This season is often a time of complexity, and people and communities experience a multitude of emotions.
On the topic of experiencing complex emotions, we will all miss our teammate Anna Rogotzke as she moves to another job opportunity at the Minnesota Department of Health with the Office of Statewide Health Improvement. She is a cherished, thoughtful member of this team. I am very grateful for what Anna has contributed to make our work come to life. We couldn't have done it without her! At the Minnesota Health Equity Networks, we pride ourselves on building relationships and connections with each other and you. Because of these connections, Anna will always be a part of the Networks.
This holiday season may stir the need for extra mental and emotional health support. We encourage you to consider what you may need to take care of yourself at this time.
Here are some ideas of ways to support yourself and the people you love:
- Ask a friend or family member to be your check-in person and or text them if you need support
- Get outside during overwhelming moments and take a walk
- Consider what has been difficult in the past, and make a plan should something similar come up again (one plan might be to remove yourself from those situations)
- Take yourself or a beloved one out for coffee/beverage to get away from stressful dynamics
- Should there be an emergency or need for emergency mental health support:
- In Minnesota, for immediate emotional or mental health support, call or text 988 to connect with the 988 Suicide & Crisis Lifeline
- The Trevor Project provides Crisis Support Services for LGBTQ+ Young People -- https://www.thetrevorproject.org/get-help/
Taking care of ourselves and those we love is one way of paving the way for future generations to live in a more caring and equitable world. Let's model this for each other in the upcoming holiday season.
With much care,
short
Coordinator's corner: Farewell from Anna
Reflections and activity highlights from the regional coordinators.
My time with the Health Equity Networks has been incredibly fulfilling. While I am saddened to step away from regional work, I'm grateful for the experiences and relationships I've built along the way. I'm excited to begin a new chapter as the Cannabis and Substance Use Prevention Grants Manager within the Minnesota Department of Health Office of Statewide Health Improvement Initiatives Division.
Over almost three years, my perspective on health equity has evolved. I've realized that health equity means different things to different people. I've learned that to truly make a difference, it's essential to meet people and communities where they are. I've also discovered incredible equity work happening in southwest Minnesota and across the state—work that often goes unnoticed or uncelebrated. The partners doing this important work deserve much more recognition for their tireless efforts.
One such organization is Horizon Public Health. They have done impressive work implementing health equity initiatives, especially through the Network's grant funding. Horizon Public Health has made significant strides in advancing equity within its own programs and has become a valuable resource for others working to create shared language and understanding around health equity. This is a great example of how localized efforts can have a broad impact, and it's been inspiring to witness the positive outcomes of their dedication to equity.
I hope the Southwest Region continues to build more connections and trust, leading to even more progress in equity work. Organizations and communities actively working together can ensure that all individuals, regardless of background or circumstance, have an opportunity to thrive. I will continue to be an active member of the Network and be involved in health equity efforts within my community and region. Although my role is shifting, I hope to remain connected to the amazing people I've met in the Southwest region and across the state.
I sincerely want to thank everyone I've crossed paths with throughout my journey. Your contributions—whether you are aware of them or not—help shape the networks and further the work of health equity in profound ways. - Anna Rogotzke
Spotlight on: Faribault and Martin County Health and Human Services
The team working at Faribault and Martin County Health and Human Services is distinctive for many reasons, including the fact that two staff members have the same first name: Kaylee Diefenderfer is the Health Communications Planner, and Kaley Hernandez is the Public Health Planner and Statewide Health Improvement Partnership (SHIP) Coordinator.
Diefenderfer and Hernandez share more than their names. They also share a passion for their work, particularly the Bridges out of Poverty training their agency provides. Funded partly by a Minnesota Health Equity Networks grant, Bridges Out of Poverty is designed to give participants a deeper understanding of poverty. It promotes empathy among staff and community members, which results in stronger relationships.
“We use Bridges out of Poverty to develop programs and strategies that improve relationships at the front-line level, improve outcomes at the organizational level, and improve systems at the community level.” – Adapted from Faribault and Martin Counties website.
In 2019, Bridges Out of Poverty became a required training for all agency staff and is now part of the onboarding process for new hires. The agency has two certified Bridges Out of Poverty trainers, Diefenderfer being one of them, which has allowed them to offer the training to the broader community. To date, Bridges Out of Poverty has been offered to schools, churches, and other community groups. Many participants have since become program champions.
“We have seen immense success! We now have an agency-wide Bridges Out of Poverty workgroup and have modified some of our processes because of what we have learned. And community members and organizations have tried and implemented practices presented on the first day of training!” – Kaylee Diefenderfer
Staff and community members learn how to navigate conversations in a way that honors the work being done and leaves space for growth into something more equitable, like the work currently spearheaded by Kaley Hernandez with SuperShelves. Two local food shelves have evolved into SuperShelves, which helps to address food insecurity and food equity issues in the region. The project makes accessing appealing and healthy food easier for community members. This achievement illustrates the success of the Bridges Out of Poverty training, the contributions of the SHIP program, the Health Equity Networks Grant, and the work of Diefenderfer, Hernandez, and their colleagues and community partners.
“The SuperShelf work goes hand in hand with food access, and to become a certified SuperShelf, you need to meet certain requirements. They include equity goals like choice, access, and creating a welcoming environment for shoppers.” - Kaley Hernandez


Hernandez is helping other food shelves take “baby steps” toward becoming a SuperShelf by focusing on more client-centered food choices and creating welcoming spaces. SHIP funds are used to purchase refrigerators and freezers with glass panels, which is recommended to promote client choice. According to Hernandez, “if or when they decide to go down the SuperShelf path, they already have some boxes checked.” One of Hernandez’s ultimate goals is to build an understanding of SuperShelves and eventually have all food shelves in the area become super shelves.
“It has been really inspiring to watch partners go from being very hesitant about becoming a SuperShelf to being ecstatic about the change and becoming an advocate!” – Kaley Hernandez
The Bridges Out of Poverty training has been a success inside and outside of the agency. Both Diefenderfer and Hernandez hope they can offer more opportunities in the future to address poverty issues and more ways for community members to participate.
“This has been an incredible process, and it feels like we are creating a positive ‘force’ within our community. The more we’ve shared about it, the more people want to learn about it, inside and outside of our counties.” - Kaylee Diefenderfer
So, how did we get here?
Reflections on the start of the Health Equity Networks from Jeannette Raymond, Public Health Practice Assistant Section Manager
This past September, Shor Salkas and I presented the Health Equity Network project to our Centers for Disease Control (CDC) Grant Manager. It was impressive to pause, reflect, and report on all the work of network participants, staff, grantees, and supporters. Here’s some of the story:
In the Spring of 2021, Kou Thao, the director of the Center for Health Equity, asked the Center for Public Health Practice and its Community Engagement (CE) Team to develop a funding proposal for a statewide equity network project. The team’s engagement and equity expertise and the section’s relationships with local and tribal public health provided a strong foundation for reaching every part of the state.
In the Summer of 2021, A CDC COVID Equity grant was awarded to build the relationships between the health equity capabilities of governmental and community-based public health organizations through regional networks and grants. The CE Team researched the components of successful networks through meetings with existing network projects and a literature review. From this, they developed a project design, position descriptions, evaluation approaches, and more.
Between the Spring and Fall of 2022, all Networks staff were onboard. In a phenomenal effort for a new project with new staff, six regional networks were launched, and the first request for grant proposals was posted.
As of September 2024, the Health Equity Networks have increased knowledge, skills, and abilities for health equity and community partnerships by generating stronger relationships, fostering new partnerships, and spurring organizational changes. 2285 people attended statewide and regional gatherings; network coordinators met with 478 partners; 1383 people participated in statewide and local trainings; 50 organizations were funded; and about 5300 people received the monthly newsletter.
My participation in developing, launching, and implementing the Health Equity Networks project is one of my “points of pride” as I move into retirement. With future funding now secured, I know we are all looking forward to what is yet to come!
May you be guided by the lessons of our past and use them to build a more equitable future
Message from Shor, Project Manager
Dear Networks communities and partners,
This is a time of change and transition, and a lot is happening with the Minnesota Health Equity Networks. For example, we are in the midst of hiring a new Northwest Regional Coordinator.
We are also saying goodbye to Jeannette Raymond, who plans to retire in mid-November. Jeannette has uplifted health equity work, community engagement work, narrative work, and my own work. She has been a true partner in creating the Minnesota Health Equity Networks. Thank you, Jeannette, for all you have done for us!
This season also brings an opportunity to connect with those who have come before. In many cultures and traditions, our ancestors return to us at this time, and we also pay homage to them. When I think of these traditions, it does not feel spooky at all. Instead, it feels like a time of connection, listening, remembering, learning, and honoring who and what has come before us.
We in the Health Equity Networks constantly look to those who have come before us, listening and learning from their stories and experiences. This informs what we are doing now and what we hope to establish for our descendants. I often tell my team that this health equity work is generational. It is an opportunity to do what we can now to create a more equitable world for our descendants to build upon.
What we do alongside our partners working in many areas of Tribal health is a beautiful example of this ongoing work. In the Networks, we acknowledge Tribal sovereignty, work to build government-to-government relationships, and strive to honor and understand the histories that have led to the moments we are in right now. We look to our leaders at the Office of American Indian Health, who support MDH in determining how to do this in meaningful ways, and we are grateful for their partnership as we all move toward healing for the future.
Take care,
shor
October 2024
"No one knows everything, but together we know a lot."
Spotlight on: Minnesota Health Equity Networks
In this month's newsletter, the Networks would like to spotlight its own efforts as they welcome new partners and celebrates two years of health equity work in Minnesota.
The Minnesota Health Equity Networks team photos reveal a lot about their approach to advancing health equity across Minnesota. Gathered in front of meaningful locations, such as in front of a mural in Mankato or by a wall sign that reads "Do the Most Good" at a community gathering space in Minneapolis, these images capture a vibrant, diverse, and united team of collaborators dedicated to their mission.
The Networks' efforts are deeply intertwined with and centered on the extraordinary organizations and communities they serve. They emphasize that each region, community, and Tribal nation faces distinct inequities and, therefore, requires tailored solutions, a belief reflected in all team communications and programming.
"Our approach with the Networks is based upon the belief that health equity is about honoring the humanity of all people. We are all responsible for making our organizations and world a better place." – Shor Salkas, Project Supervisor

The Networks began in 2022 in response to COVID-19 and the heightened awareness of the successes and inequities made more visible across Minnesota by the pandemic. The Networks focus on three main action categories that promote health equity: connect, strengthen, and amplify. Network coordinators live in the regions that they serve and share an understanding of the residents' lived experiences and realities.
"I am alternately shocked by the health disparities in my region and amazed by the strength and wisdom we possess. Meeting with those working in public health, whether that be a county agency or a community organization, is always an honor and a learning experience for me." - Mary Mitchell, Northwest Regional Health Equity Networks Coordinator.
Network coordinators host quarterly gatherings on relationship building, community issues, connection, and collaboration relevant to the region. The Networks team also offers ongoing statewide gatherings centered on topics such as disability justice, community involvement, and shared language. The Networks customize coaching and training for Network partners based on their requests.
“I love knowing that, while some people see us as the leaders in equity efforts, in reality, we work alongside our partners. We are growing and learning about health equity together." - Anna Rogotske, Southwest Regional Health Equity Networks Coordinator.
Network coordinators engage with partners one-on-one, providing referrals and resources while celebrating successes and addressing challenges. Spotlights during gatherings, trainings, and newsletters amplify health equity efforts from initial planning stages through implementation and evaluation. Storytelling has proven to be an effective method for promoting health equity and fostering empathy, making narrative a central component of the Networks' work. Encouraging organizations to share their health equity stories has become a key element in networking and connecting partners.
"I have learned so much from the stories that have been shared by our partners in the spotlights. They really reinforce the fact that effective and creative health equity work is being done in Minnesota." – Colleen McKinney, Northeast Health Equity Network Coordinator.
Above all, the emphasis is on listening and learning. One of the Networks’ baseline assumptions is that "no one knows everything, but together, we know a lot." As part of this, the Minnesota Health Equity Networks team is requesting input and suggestions from newsletter readers and community partners on training that might be helpful and what else the Networks could do to help advance health equity across the state. Input can be shared here: Minnesota Health Equity Networks Connections – Future Training Requests
“We are working to plan for the next two to three years and brainstorm what the Minnesota Health Equity Networks could look like and feel like. As always, we don't want to do this without you.” – The Minnesota Health Equity Networks Team
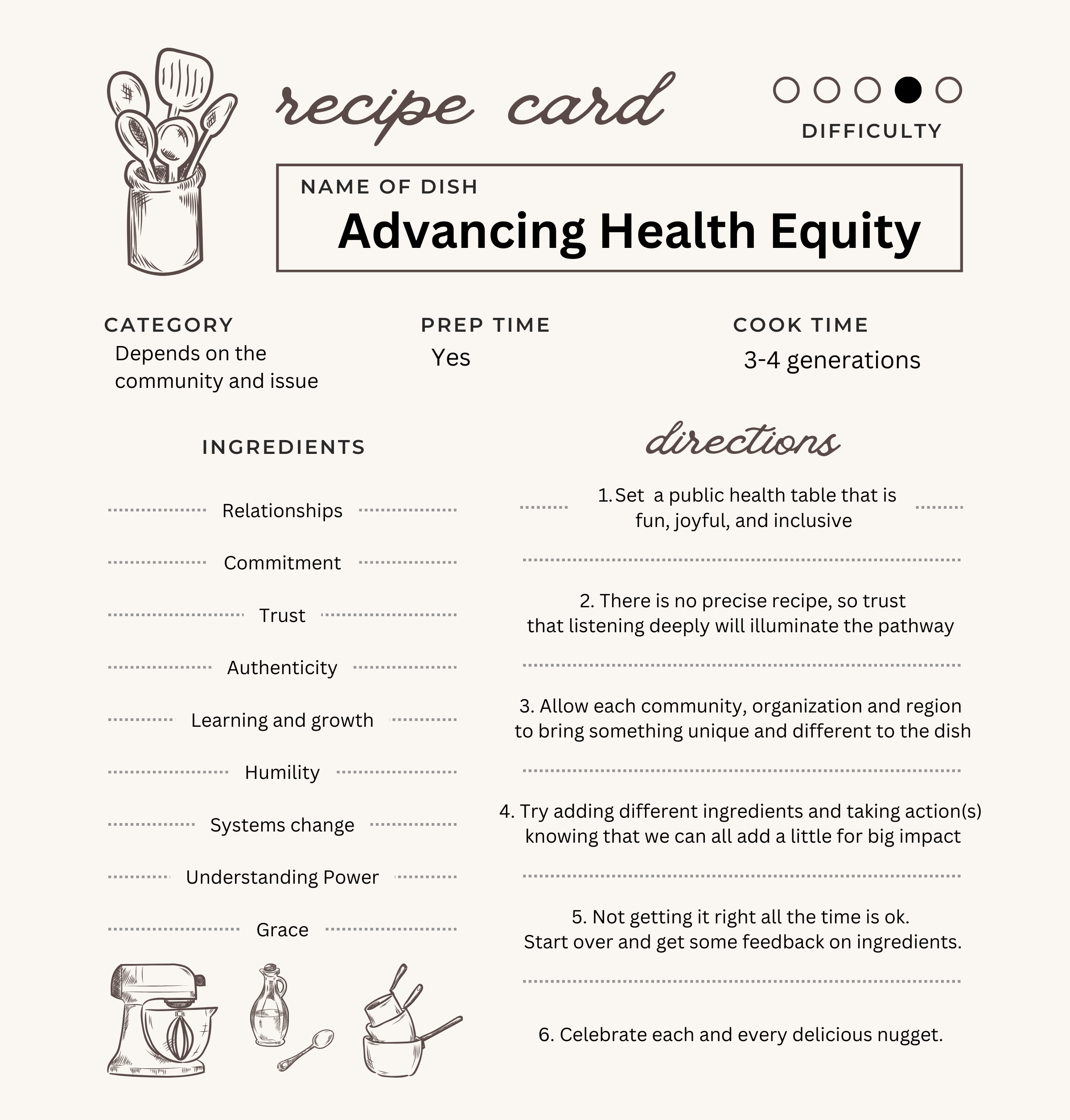
What's in a recipe for health equity?
Message from Shor, project supervisor
Our team at the Minnesota Health Equity Networks has been deeply engaged in discussions about our vision and future work, imagining what the next few years will bring. These conversations have been both productive and enjoyable. One particularly inspiring discussion led us to envision advancing health equity as if it were a recipe for a dish or even a full meal. We began considering the essential ingredients and the steps required to achieve health equity.
The coolest part of this process was realizing there’s no single right way to make this “meal.” The recipe needs constant adjustment, and sometimes, our efforts don’t yield the desired outcome. When that happens, we reflect on the ingredients or steps that impacted the result and then start again.
We brainstormed some ingredients to include on our recipe card (see below). What else could be included? What ingredients are missing? What directions do we need to add? What has worked well for you?
Thanks for adding to our collective recipe with us,
Shor
Building upon strength and culture
Spotlight on: Comunidades Latinas Unidas en Servicio (CLUES)
Vibrant colors and beautiful images greet visitors even before they enter the Comunidades Latinas Unidas en Servicio (CLUES) offices in St. Paul. Outside the light-filled lobby, a mural features a young girl draped in a shawl decorated with flags of numerous Latin American nations that the people of CLUES represent. Embedded within the symbolic design, a banner holds the text, “La Cultura Cura,” or “Culture Heals,” in English.
The CLUES building in St. Paul houses the Mexican Consulate, offices for the Abriendo Caminos Behavioral Health Department, space for cultural art exhibits, and a commercial kitchen set up for the weekly food distribution known as the “Canasta Familiar” or “Family Basket.” Color, art, and culture fill the space and surround anyone who enters.
“When people come to CLUES, we want them to feel welcome and at home. Here community becomes family. “ – Jessica Pleguezuelos, Senior Director of Marketing and Communications, CLUES

CLUES was founded in 1981 on the west side of St. Paul by Latino social workers, including Rafael Ortega, who is now a Ramsey County commissioner. Now celebrating 43 years with offices in St. Paul, Austin, Willmar, and Minneapolis, CLUES has 145 staff members and plans to add more when funding allows.
CLUES offers various services, including those that address food insecurity, community health and wellness, housing stability, early childhood, cultural engagement, employment assistance, adult education, youth services, and more. According to one of their brochures, “CLUES programs are designed to provide access to resources and opportunities for Latino families and individuals to lead healthy and thriving lives.”
“Providing a sense of belonging and support networks is at the heart of who we are. We then provide targeted services or interventions as opportunities for transformational impact.” – Ruby Azurdia-Lee, President and CEO of CLUES
Ruby Azurdia-Lee, the president and CEO of CLUES, came to the United States from Guatemala the same year that CLUES started. Ruby tells the story of the learning process she experienced when hoping to buy a house and the cultural differences between the United States and Guatemala regarding establishing credit and financing. She understands the immigrant experience because she lived it. That’s part of the reason CLUES staff provides holistic services and support with navigation of systems and resources.

“CLUES advances social and economic equity and wellbeing … uplifting individuals and families, and activating leadership for systemic change.” – Portion of CLUES Mission Statement
Since 2019, staff in their Behavioral Health Department (“Abriendo Caminos,” or “Breaking Ground”) has more than doubled to forty-five with hopes of adding twenty more employees in the future. In May 2024, CLUES officially became a Certified Community Behavioral Health Clinic (CCBHC). This certification is a milestone for CLUES and the Latino community in Minnesota. Beyond this impressive accomplishment, they maintain a goal of providing services to all regardless of insurance status. Senior Clinic Director Benjamin Feigal explained that they constantly work to expand all behavioral health efforts and capacity.
With awareness that close to fifty percent of Latinos in Minnesota are under the age of 20, CLUES collaborates with Best Buy to connect young people to technology and the careers of tomorrow. The Best Buy Teen Tech center is adjacent to the main floor of the CLUES St. Paul location and features professional-grade equipment that lets teens make, create, and innovate while learning skills that can be used in school, careers, and beyond. Career pathways program internships are also available.
Prosperity and economic development are also a focus of CLUES's work, with a pilot project just beginning that is described as a “business incubator for Latina women.” Informal daycare providers can get small business training, licensing, and certification training and have options to rent daycare sites in the former Head Start building just down the street from CLUES in St. Paul.
These opportunities have not been achieved without challenges. Many community members are uninsured or underinsured, and funding inequities are still prevalent. The goal for the future of CLUES is long-term sustainable partnerships with public and private funders so that they can offer financial stability and continuity for both community members and staff.
“Access continues to be the barrier. For us, access for all IS equity. “ – Ruby Azurdia-Lee
Let's create systems that heal, not harm
Message from Shor, project supervisor
I share a message with you each month in this newsletter, but this month, I'm going to tell you about myself in a different way.
Over the last two and a half years, I have supervised the Health Equity Networks team. It's been such a dream. I came into this role with many years of coaching and training in public health departments and coalitions, helping people advance health equity and practice community engagement in ways that are as unique as each community. This work is built upon my commitments, values, and the stories and experiences that have shaped them.
My grandparents and parents came to the U.S. as refugees to seek a life with more opportunity and less discrimination than what they were facing as Jewish people in the former Soviet Union. Frequently, my mother said that she came here so that her kids could have a better life - one free of oppression. Unfortunately, as a queer, transgender, neurodivergent, and disabled person, I have also experienced a great deal of discrimination and oppression. These experiences fuel my work. I know we can better create systems that heal rather than harm.
I deeply believe that we owe it to our descendants (and ancestors) to imagine a world where every person can be free, cared for, and loved. This can be achieved not just interpersonally or communally but systemically. It is the basis of health equity work for me. We all deserve to live our lives with dignity, kindness, and respect.
Will you join me in seeking this world?
-Shor
Coordinator's corner
Reflections and activity highlights from the regional coordinators.
'Tis the season of fall transition! The Networks' Metro Regional Coordinator, Lil Pinero, has taken a new position within the Minnesota Department of Health doing youth substance misuse work. The Networks team is excited for Lil, and we will miss her on our team. With Lil's transition, we've been discussing how we can serve the Metro in her absence. If you have thoughts about this or how the Networks can best serve any region, please reach out to a regional coordinator.
We value your input, as we are always working to build out programming that is reflective of your needs and ideas.
In solidarity,
The Minnesota Health Equity Networks team

Network member spotlight: WeARE - The Clinic (Brainerd, MN)
View the full July newsletter: Minnesota Health Equity Networks July Newsletter
Tucked in the middle of a strip mall on Oak Street near downtown Brainerd, WeARE – The Clinic boasts cheery bright green and purple signage. It's across the street from the Brainerd Family YMCA and about a block from the local high school. Welcoming and approachable, WeARE is the go-to resource for compassionate and inclusive sexual health care, transformational health education programming, and collaborations that serve reproductive justice in the Brainerd Lakes Area.
“Success happens every day at WeARE. We love creating the space for folks to ask questions, make their own medical decisions, and leave feeling taken care of and confident about their sexual health.” – Devon Charlier, Executive Director, WeAre - The Clinic

WeARE, which stands for Advocates for Reproductive Education, was formed in 2015 out of concern for high unintended pregnancy rates in Crow Wing County. The four women on the founding board, Becky Twamley, Susan Hadland, Julie Ingleman, and Cindy Moore, brought a wide range of skills and knowledge to the founding of WeARE, including expertise in women's health, global health, public health, pharmacy, reproductive health, marketing, and social service.
While WeARE’s initial focus was education, the clinic opened in October 2017, providing comprehensive reproductive health care services to the Brainerd Lakes Area and beyond. By 2018, they had over 300 patient visits. Five years later, in 2023, they had over 780 visits and more than 500 returning patients. WeARE also has longstanding partnerships with Central Lakes College and the Relationship Safety Alliance and operates outreach clinics to further serve community members. The WeARE education program, Let’sTalk, has also grown to meet the massive need in the community for evidence-based, medically accurate, inclusive, and developmentally appropriate information about sexual health, healthy relationships, consent, and identity. It reaches community members over 2,000 times annually.
“Positive youth development is foundational to the work done at WeARE. This means that we feel that young people are capable of making decisions, and they should be involved in decision-making processes.” – Devon Charlier
WeARE has an active Youth Advisory Council (YAC), and young people are deeply engaged in the organization's work. Authentic youth-adult partnerships are created and maintained. According to Devon, the key to positive youth development is a “strengths-based approach instead of a deficit-based approach."
"Youth have many strengths and are important members of our society. They care about what is going on around them and need to know that adults want to support them in their growing independence and responsibilities." - Devon Charlier
Devon defines reproductive justice by quoting a study, "Reproductive justice considers the ways that socioeconomic status, gender, and race shape reproductive health care experiences and health policy." That definition includes the right to have children, not to have children and to parent in safe and supportive environments.
"At WeARE, we work to integrate the reproductive justice approach into all that we do.” - Devon Charlier
When community members expressed a need for support to the parents and family members of folks with or exploring transgender nonbinary gender identities, WeARE offered support groups. They also asked for feedback, which revealed the need to build an increased level of trust and engagement with community members who are trans, nonbinary, and gender nonconforming. WeARE plans to continue to adapt its efforts to offer support through feedback from paid listening sessions. Using that input, they hope they can better support the entire regional community with WeARE’s education and health care services in the future.
“A further challenge is that we are living in a time of unprecedented levels of hate and violence toward folks with marginalized identities, coupled with intensifying restrictions on access to reproductive and sexual health care while rates of sexually transmitted infections (STIs) and unplanned pregnancies, especially among young people, continue to rise.” – Devon Charlier
It hasn't all been easy. WeARE experienced several roadblocks since its founding, including space, funding, and staffing challenges. They rely on state and foundation funding and generous individual donors to ensure they can serve each person who walks through their doors. Unfortunately, due to a lack of medically accurate reproductive and sexual health education and resources for students and people of all ages in communities like Brainerd, there is significant stigma and shame that surrounds the idea of sexual health. This has prevented many local funders and individuals from publicly supporting their work. As WeARE continues to provide needed services, they seek more support through funding opportunities, volunteers, and donations while adapting their strategies to meet the needs of their community.
“Our goal is to care for more patients and educate more people each year, and ultimately create a culture change across our community that is conducive to everyone thriving. Our focus keeps us grounded and connected to what's most important – serving the health and wellbeing of those who need us most in our region.” – Devon Charlier
Listening to what youth and community want and need
Network member spotlight: CornerStone Community and Youth Center (Frazee, MN)
View the full June 2024 newsletter: Minnesota Health Equity Networks June 2024 Newsletter
The lower level of the CornerStone Community and Youth Center in Frazee, MN, is a hive of activity. A 40-foot chalk wall, a pool table, ping pong, foosball, TV, and gaming offer artistic creativity and fun. In the Maker’s Space, youth can cook and eat in a full kitchen, with a pantry and cupboards full of ingredients for budding young chefs and cooks. They can learn to make t-shirts, woodworking, painting, sketching, and pottery. Youth can operate equipment like 3-D printers, laser engravers, Cricut Maker 3, and screen printers. Offered to youth from 4th to 12th grade as a free drop-in center, community members and families can join the Center and, with a membership, can take advantage of these opportunities outside of regular operating hours.
“It's wonderful chaos. And when you walk in there, no one is on their phone." - Karen Pifher, Co-Owner of Creative Community Consulting.

CornerStone Community and Youth Center was founded and built on the voices of local youth with the goal of improving mental wellbeing in the community. In 2019, Essentia Health completed a community needs assessment, which showed that the top concern in the community was youth mental health. Youth focus groups identified root causes: youth didn't feel cared for, had no safe place to gather with friends, eat together, or be involved in meaningful activities outside of school sports. Teens were asked to describe "the best place to be a kid" and illustrate their ideas through brainstorming and creating a community map. The process was repeated with adults. A steering committee of stakeholders from churches, schools, and community groups worked to develop a vision ever since.
They began in small ways. Community members created a mural in town, they launched community events, and youth created window art. At the height of COVID, a church showed drive-in movies. Though these efforts were successful, it soon became evident that a nonprofit youth center was badly needed, and income to support the Center would be required. A local church offered to donate its building, and the site for the CornerStone Youth and Community Center was established. The building needed a complete renovation; volunteers did 90% of the work through a grassroots effort. Planning and design specifics were based on input from children and youth in the community. Despite unforeseen delays, repairs, and expenses, the doors to the lower level opened in the spring of 2023.
“You start getting momentum, and one success leads to another. Things just keep growing!” - Karen Pifher.
Noting that Native American youth and LGTBQIA2S+ youth experience greater health disparities, CornerStone received Health Equity grant funding to learn how to support the wellbeing of these youth culturally, environmentally, and in other ways. A Native American cultural committee identified specific goals, including language immersion, cultural training, and access to Indigenous art and ceremony. When asked, LGTBQIA2S+ youth said there was a clear need for staff training in the school - so an LGTBQIA2S+ mental health professional provided education to all high school employees. Additionally, policies were updated to support diverse youth and cultural beliefs.
To date, 300 school-age children have registered, and 200 volunteers have contributed to the Center's success. Each day, about 40 to 50 youth attend the Center. In June, the second-floor bistro opened for business. The facility will be sustainable by implementing a coffee and crepe bistro, retail and gift shop, maker's space, performing arts, and space rental.
“We have very important things in place: a governing board, a sustainable and investigated business plan, ongoing income sources, and qualified individuals to build the organization.” – Adapted from CornerStone Community and Youth Center website.
CornerStone staff hope to hire an on-site Indigenous cultural lead to continue building connections and engagement with youth and coordinating activities. There is also discussion about a possible Family Resource Center. Above all, they will work to reach those they haven’t reached by continuing to listen to what is wanted and needed in the community.
CornerStone Community & Youth Center is not just a building; it's a lifeline for our community. – Cornerstone Community and Youth Center Website
Making human-to-human connections
Network member spotlight: Zumbro Valley Medical Society Foundation Street Medicine Program (Olmsted County, MN)
View the full May newsletter: Minnesota Health Equity Networks May Newsletter
Three years ago, Zumbro Valley Medical Society (ZVMS) started a Street Medicine program. This program brings together physicians, medical students, community partners, and individuals with lived experience to identify and create effective ways to improve health care for people experiencing homelessness in Olmsted County.
We need to adapt to people and their circumstances rather than expect people to adapt to us.” – Beth Kangas, Executive Director, ZVMS
During “street rounds,” a physician and medical student join a county social worker to visit people living in encampments, under bridges, and on street corners to identify the medical and social services they need.
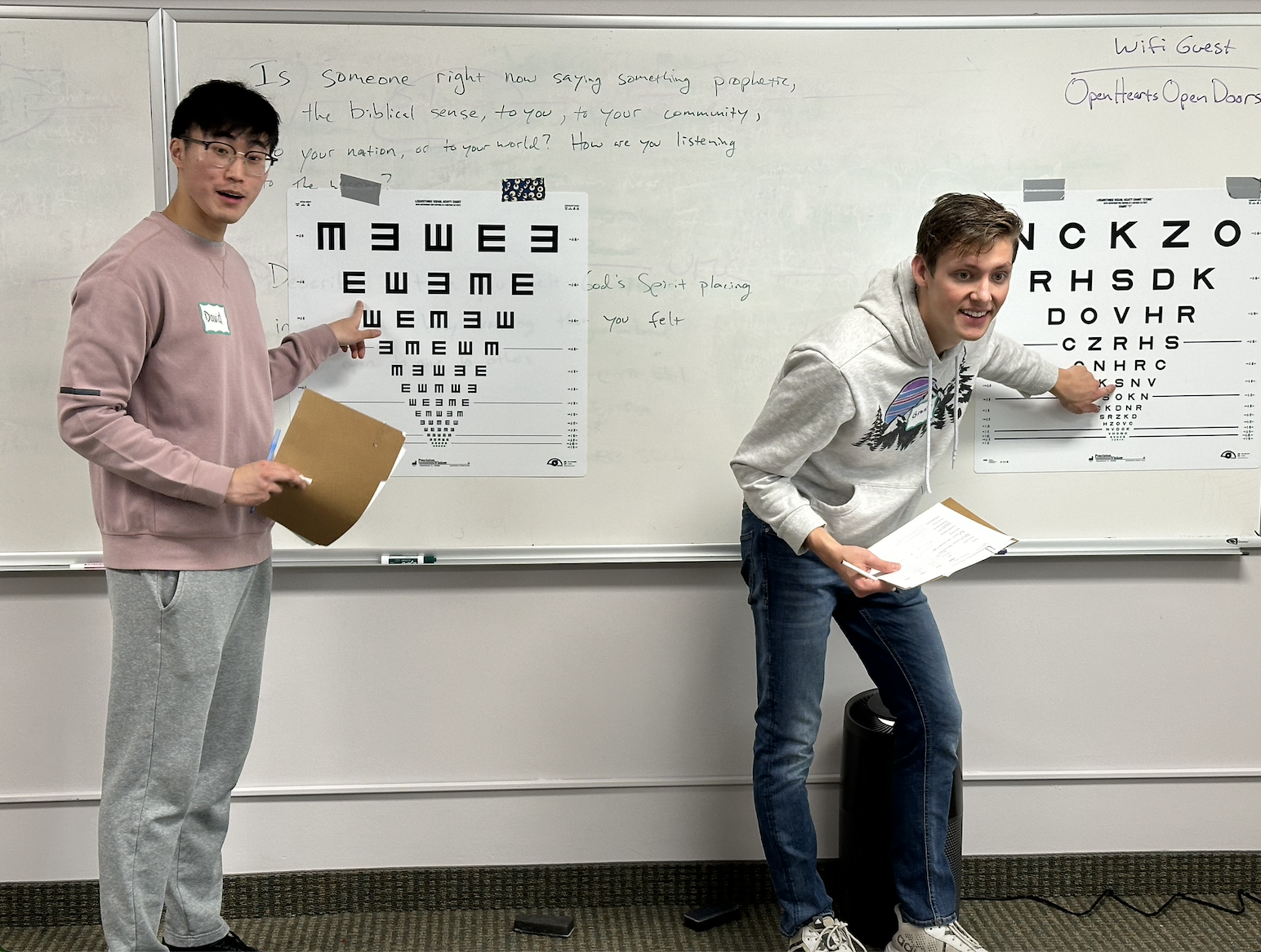
Collin’s story shows how street rounds can go beyond health care for the people it serves. A year ago, Collin fell off a bridge and injured his head and knee. His choices were to go to the emergency department or return home, which at the time consisted of two shopping carts and a blanket. He opted for home. The next day, the street medicine team visited him, examined him, and gave him bandages and pain relief. Two months later, he attended a one-day community meeting that ZVMS Street Medicine was holding to learn about people’s experiences with medical care. Since then, Collin has helped ZVMS Street Medicine design and facilitate projects. Soon, Collin will have an apartment of his own and will continue to collaborate with ZVMS Street Medicine as it moves forward. His lived experience and knowledge about housing insecurity make him a valued team member.
ZVMS Street Medicine takes a three-pronged approach to addressing health inequities:
- Provide direct care to people in their own environments through street rounds and community clinics;
- Train the medical community to provide high-quality, compassionate health care outside of traditional clinical settings;
- Advocate for changes in systems and processes that affect the health care that people receive.
Community clinics begin with concentrated one-day events, such as a foot care clinic. The skills and supplies are then dispersed to smaller drop-in clinics at additional locations, such as weekly foot soaks at Dorothy Day Hospitality House. ZVMS Street Medicine also held two eye care clinics in 2023 that served close to 250 people, along with a dermatology clinic in April of 2024. Another eye care clinic is planned for June of 2024.
“This kind of work helps avoid physician burnout. They can prioritize everyone’s humanity more than a system.” – Beth Kangas
ZVMS Street Medicine also offers a Street Medicine optional elective for first-year medical students at Mayo Clinic Alix School of Medicine (MCASOM). Two-thirds of the current first-year class of future physicians participated this year. In addition, Street Medicine content has been added to the MCASOM curriculum.
ZVMS Street Medicine is currently implementing two other programs. One aims to improve the medical discharge process for patients experiencing homelessness. The second project draws on people with lived experience of homelessness and hospitalization to create guidelines for the development of recuperative care (also known as “medical respite”) in Olmsted County. The project will serve unhoused patients who are discharged to “home,” but need a place other than a tent or overnight shelter to heal.
“We put a lot of work into educating people, reducing stigma, and making human-to-human connections. In this way, we can address stereotypes and work together to find solutions.” – Beth Kangas
Network member spotlight: Meeker-McLeod-Sibley (MMS) Community Health Services
View the full April newsletter: MN Health Equity Networks Newsletter
Meeker-McLeod-Sibley (MMS) Community Health Services has been working on data-driven health equity initiatives for almost a decade. However, their current work stems from a data gap realized through their most recent Health Equity Data Analysis (HEDA). HEDA focuses on identifying health inequities among specific groups. The analysis showed that Hispanic residents were underrepresented in their area’s data collection.
MMS staff responded by ensuring that the questions used in the HEDA tool were translated and culturally appropriate. They considered the cultural connotations of the tool’s word choices when conducting the survey. The staff collecting responses worked to establish trusted relationships with the Hispanic community with the goal of collecting the most accurate data possible and connecting with community members who might not otherwise participate.
“We’ve had a great response from community members in learning and growing together.” – Vlada Gladis, Health Educator, Sibley County Public Health and Human Services (Meeker-McLeod-Sibley CHS)

Photo of Meeker-McLeod-Sibley Community Healthy Services staff. Photo courtesy of MMS CHS.
Through these conversations, MMS staff deepened their understanding of the Hispanic community and the health barriers its members often face, such as poor nutrition, limited exercise options, language barriers, immigration status, access to and quality of health care, transportation, mental health issues, and racism.
“We were able to learn a lot about the Hispanic members in our communities. For example, that Hispanic is the preferred term when describing and referring to the culture.” – Vlada Gladis
MMS staff understood that to create lasting connections and improve their data, they had to include the community in the entire process. They took the time to follow up, share results, and ask if there was any other information to give. Vlada said that they consistently focus on making sure that when staff connects with a community member, that connection is beneficial for all parties in the present and into the future.
Using Regional Healthy Equity Network Grant funds, the MMS Community Health Services focused on building community connections and educating the public on health equity. They have organized events and led discussions on how to address community needs. MMS Community Health Services recently sponsored a “Bridges Out of Poverty” workshop, which will be followed by more training for community stakeholders. Dr. Terry Wu presented information on the neuroscience of belonging in his presentation of “Us vs. Them,” and MMS will soon host a Poverty Simulation event in partnership with United Community Action Partnership (UCAP).
“At each event, we learn of more members in the community who have the desire to collaborate to advance health equity.” – Vlada Gladis
Vlada says, “We are striving to develop a network of these amazing individuals who can collectively move our communities forward.”
The project also includes building connections with other cities and counties where collaboration already has established momentum. They plan to continue gathering information from community members and use it to create a framework that addresses needed change.
“We’re planning to give individuals from all backgrounds seats at the table. We hope that individuals will share their insights, contribute in a way that they find meaningful, and create bridges to meet the needs in our communities.” – Vlada Gladis
Network member spotlight: Arrowhead Area Agency on Aging
View the full March newsletter: MN Health Equity Networks March 2024 Newsletter
As people age in our society, they can become marginalized. The Arrowhead Area Agency on Aging, or AAAA, encourages the development of age-friendly cities and counties where older adults are integral parts of their communities. AAAA’s message is that older adults should have opportunities to contribute and be active, engaged and connected. The Agency offers a breadth of services, working in many ways to keep aging adults involved in creating vibrant communities.
“Changes can be made in big or small ways. Central to our work is reframing the way we talk, think, feel, and act about aging.” - Georgia Lane, Aging Services Planner, Arrowhead Area Agency on Aging
One of the many successful projects organized by AAAA is the Arrowhead Changemakers. Changemakers serve as ambassadors to promote meaningful, lasting changes that help their communities become better places to grow up and grow old. There were sixteen active Changemakers in 2023, and a second cohort launched this month.

Photo of Changemakers visiting with community members. Photo courtesy of AAAA.
"We seek local community members and leaders who have a passion for impacting decisions that enable people to age successfully in their communities and advocate for the needs and wants of older adults." – Recruitment information for Arrowhead Changemakers
Changemakers embrace positive attitudes about aging, which can enhance the quality of life and foster stronger and more inclusive communities for all ages. Changemakers are critical in bringing localized issues and experiences to AAAA, the Governor’s Council on an Age-Friendly Minnesota, and other leaders and organizations. These contributions spark conversations on ending ageism and championing an age-friendly Arrowhead region that respects, honors, and celebrates individuals at every stage of life.
“An age-friendly community (or state) is one that enables all residents to thrive at every age and life stage.” – AAAA website

Photo courtesy of AAAA.
As a state-designated Area Agency on Aging serving Aitkin, Carlton, Cook, Itasca, Koochiching, Lake, and St. Louis counties, AAAA is responsible for developing a coordinated and comprehensive system of services for older adults and their family caregivers. To help accomplish this goal, AAAA awards grants and contracts to agencies for services that enrich the lives of older adults and their family caregivers. The Agency partners with community organizations to address issues like transportation, meals, health promotion, caregivers, respite, and chore services.
From developing age-friendly communities to providing referrals and assistance through the state's Senior LinkAge Line, the Agency advocates for statewide policies that promote healthy aging and offers informational and wellness classes throughout the Arrowhead region. AAAA planning staff works to address service gaps in the region, support partner organizations, and advocate for aging services.
“What we are doing is a great example of health equity in action. We are listening to the voices of people who are plugged into their communities, and educating about how older people think, talk, and feel.” – Georgia Lane
Network member spotlight: The Annex Teen Clinic
View the full February newsletter: MN Health Equity Networks February 2024 Newsletter
Feelings of welcome and acceptance are tangible the moment one enters the Annex Teen Clinic in Robbinsdale, Minnesota. The clinic provides sexual health services and education to youth in Hennepin County and North Minneapolis.
“We try to make sure all young people feel seen and valued at all touchpoints, whether in the classroom, community, or clinic,” - Khadijah Cooper, Director of Sexuality Education
The organization began in 1971 in response to youth voicing a need for better sexual health services, especially STI testing and treatment.
"As a teen, I went to the Annex [in the 1990s] for testing during a really scary time. It was great to have a resource that I could access confidentially. While I was there, I also got some really valuable counseling advice.” – Former clinic patient
Later, the Clinic evolved into an independent nonprofit, offering comprehensive sexuality-related health services. Youth input has always guided program development, with staff aiming to empower young people to manage their sexual health.
The Annex Teen Clinic provides testing and treatment for STIs, HIV, and other conditions. It offers birth control, emergency contraception, all-options pregnancy counseling, pre-exposure prophylaxes, annual exams, breast exams, and chest exams. The lobby area is designed so young people can pick up condoms and other sexual health products without questions or paperwork.
"If I would not have had Annex, I would be pregnant and have multiple STDs." – Clinic patient
"Having access to health care changed my life because it helped me get educated on a lot of thing[s], such as sex, STI and [routine] checking. Sometimes you don't feel comfortable talking about things with your guardians or parents, so it is great to have Annex around." - Clinic patient
All services are confidential, fact-based, non-judgmental, and inclusive, and telehealth is available when possible. Service costs are controlled, and discounts are offered to patients. Khadijah said this model benefits clinic patients more than just financially.
“Young people want to pay for their services. It gives them a confidence boost, helps their mental health. They are learning to navigate the health care system for the first time. And we are setting the precedent that they have the right to advocate for themselves and make informed decisions,” said Khadijah. “It’s transformational!”
Photo courtesy of Annex Teen Clinic website.
Many teens have been coming to the Annex Teen Clinic for years, and they appreciate the clinic’s quality of services and staff.
"I have been coming here for four years for birth control, STI testing, pap smears, etcetera, and I always feel so safe and comfortable with the incredibly friendly staff. Thank you for making these appointments so easy and non-judgmental." - Clinic patient
The Annex also provides annual education on topics like STIs, gender identification, sexual exploitation, and mental health. It educates parents and professionals in schools and community settings, too.
"You guys have been helping me navigate my sexual health since I was 15. I love it here and hope you continue to help young adults. I was introduced to y’all at Cooper High School, and y’all need to continue to visit schools and educate our youth!" – Clinic patient
Annex has been able to expand services with a newly remodeled, onsite lab. Additionally, with the support of Health Equity Network grant funding, the Annex Teen Clinic is working to reach more youth through enhanced marketing efforts. Staff magnify their health equity efforts by focusing on reproductive justice and intersectionality.
After over 50 years, the Annex is still pursuing its vision: The Annex will create a community where all young people have the resources and support they need, allowing them to successfully make the transition from adolescence to adulthood.
"It gave me the opportunity that a lot of women across the world don’t have. I feel empowered to make choices surrounding my life and sex life." – Clinic patient
For more information about the Annex Teen Clinic services and parent and professional learning opportunities, visit their website at annexteenclinic.org.
A bridge to community solutions
Network member spotlight: Central Minnesota Alliance
View the full January newsletter: MN Health Equity Networks: Jan 2024 Newsletter
The Central Minnesota Alliance (CMA) began in 2018 with informal coffee meetings between the Stearns County Public Health Director and the Centracare Community and Government Relations Director. Today, the CMA is a partnership involving staff from Benton, Sherburne, and Stearns Counties, and Centracare (formerly St. Cloud Hospital.) The CMA conducts the region’s community health need assessment and community health improvement Plan.
;“We discovered that we had so much in common. It is good practice to do this work together.” – Peggy Sammons, Public Health Planner, Sherburne County Health and Human Services
Many county staff have long histories of personal and professional collaboration and cooperation. In some cases, they moved from county to neighboring county or from one position to another, maintaining positive connections that are a basis of the partnership’s success.
St. Cloud has a unique geography in that it lies within three counties: Benton, Sherburne, and Stearns. St. Cloud is the county seat of Stearns County. Benton and Sherburne’s county seats are in Foley and Elk River, which are quite a drive from St. Cloud. In response, CMA operates on a “no wrong door” approach that makes services more accessible to regional community members, removes duplicative efforts, and allows staff to collaborate.
“The key part of all of this is that we voluntarily agree to work together. It’s nothing official, nothing legal. We are driven by our desire to collaborate.” - Peggy Sammons

Photo of Health Festival in St Cloud, featuring 10 CMA Staff in front of the Sherburne County Wellness Bus.
The CMA Process Managers Team, comprised of representatives from partner agencies, shepherded the process of identifying priorities. According to Sammons, it involved many internal discussions, partnership meetings, community input, and some challenges.
“We had to be willing to have hard conversations, but authenticity and the work behind it is important.” - Peggy Sammons
Currently, the top priorities for CMA are “building families” and “mental health.” Through the most recent community health needs assessment, four “drivers of inequities” have also been identified as areas of focus for the CMA, including: Data access and systems; Structural racism and community power; and Lived experience Historical context.
“Our community partners say that our goals and drivers really resonate with them. It has enriched how we do our work.” - Peggy Sammons
To date, the CMA has conducted two community health needs assessments and two corresponding community health improvement plans. The CMA continues to build upon each effort, with the next assessment starting later this year.
“The CMA allows for a regional approach to planning, and we are seeing how our community health improvement plan is intertwined in many things that we do. This allows for capacity building and really expands our collaborative reach. - Jaclyn Litfin, Community Health Services Administrator, Benton County Public Health
2023
Cooperation, not competition
Network member spotlight: Community Resource Connections
View the full December newsletter: MN Health Equity Networks Dec 2023 Newsletter
Ruth Sherman approaches her work at Community Resource Connections (CRC) with inspiration from her late father, a dairy farmer. He organized cooperative farming with his neighbors, sharing equipment and working collaboratively in the small rural community where Ruth grew up.
“We need to be cooperative, not competitive. When agencies know and trust each other, clients benefit. It’s the people who participate in this process that make things happen. If others didn’t share that mission, we’d be spinning our wheels.” Ruth Sherman, Executive Director, Community Resource Connections (CRC)
Ruth says CRC’s mission is to provide access to services that allow people to improve themselves and the lives of those around them. She adds that when CRC was founded in the 1980s, nonprofits were often pitted against each other for service contracts. That type of competition led to a lack of collaboration, low staff pay, and short-term thinking. Above all, clients were not getting all the services they needed. CRC formed to change that, and still works to prevent “silos” among agencies.
Now, with offices in four counties, CRC serves as a referral source to help community service agencies reach their intended clients. One of CRC’s community offerings is an up-to-date resource directory. Member benefits include event facilitation, group marketing, consulting, and regular email communication. Ruth’s father’s vision of cooperation and collaboration continues to guide their work.

Bemidji Chamber Ambassadors congratulate Executive Director Ruth Sherman on the new location of Community Resource Connections. Photo courtesy of the Bemidji Chamber of Commerce.
“What has kept me here is that this has been a place where I can interact with the public every day – helping facilitate service education and engagement – while still impacting the larger system of services by networking with agencies, pulling them together in conversation, engaging them in collaboration to improve services to clients. When agencies get together, the results are just magical.” – Ruth Sherman
CRC’s journey hasn’t always been easy. Budget problems required creativity in fundraising to keep CRC going. In 2003 they struggled out of a $35,000 debt, using a variety of approaches, including planting plastic flamingos in community members' yards. But even those challenges had some positive results. Ruth says the situation helped the organization “clarify who we intended to be.”
Ruth came to CRC with a wealth of experience, working at Blackduck Resource Center (formerly Bemiidji Area Council of Nonprofits) and the County Child Protection System. She started at CRC feeling the need to reach out to families and individuals before problems became crises.
Ruth believes that recognizing disparities and looking beyond the surface of every situation is critical to the health and well-being of every agency and every person. She says that understanding equity and inequity is absolutely vital and is a constant learning process.
“I didn’t set out to form or participate in a program that “ensures health equity”. I chose to join an organization that affects people and systems. As providers, I believe it is our job to recognize the privileges and disadvantages that society has handed to people. We are each responsible for ourselves and for others.” - Ruth Sherman
Horizon Public Health revitalizes its health equity efforts
Network member spotlight: Health Equity Action Team (HEAT) at Horizon Public Health
View the full November newsletter: MN Health Equity Networks Nov 2023 Newsletter
In July 2022, Angie Hasbrouck and Amanda Schueler of Horizon Public Health and staff from Horizon’s program areas began a collective effort to revitalize their Health Equity Committee.
“We wanted to bring the committee back and have clear objectives around the health equity priorities of the agency.” - Angie Hasbrouck, Health Educator, Horizon Public Health
Horizon Public Health is located in West Central Minnesota and serves Douglas, Grant, Pope, Stevens, and Traverse Counties. The organization is invested in community work and provides many services to the region.
The internal committee adopted a new name, the “Health Equity Action Team” (HEAT), and rewrote the organization’s health equity policy. HEAT updated its language to reflect new knowledge about health equity, including a full set of terms creating shared vocabulary and understanding within the agency and community.
"Everyone started with a different understanding of Health Equity. If we are able to say what it is and what it means to us, it changes the whole conversation." – Angie Hasbrouck
Horizon Public Health also revamped its mission, vision, principles, and strategic goals, making health equity a guiding practice.
“With updated policy, mission, and strategies, we can direct our work and intentionally use an equity lens in all we do.” - Angie Hasbrouck
The Minnesota Health Equity Network awarded HEAT Round One and Round Two funding to support their project activities. HEAT hosted listening sessions with community members, and over 100 people participated, significantly exceeding their goal of 25. “We created processes to hear from community members and are welcoming people with lived experience [to take] a seat at the decision-making table,” said Hasbrouck.
HEAT has a renewed focus on data disaggregation, which breaks down data in different ways to be looked at with a new lens. This has helped HEAT identify trends and inequities and improve their targeted work plans.
HEAT plans to conduct five more listening sessions and dive deeper into how their data can be used to engage the community.
“Horizon’s goal is to continue to build capacity around their Health Equity Action Team and encourage the group to be a driving force behind their health equity initiative.” -Angie Hasbrouck
In September 2023, Horizon Public Health received the Inclusive Workforce Employer Designation from the Rural Minnesota Concentrated Employment Program (Rural CEP) and the Minnesota Department of Employment and Economic Development (MN DEED).
Addressing the health inequities Latine people encounter
Network member spotlight: Communities Organizing Latino Power (COPAL)
View the full October newsletter: MN Health Equity Networks Oct 2023 Newsletter

Communities Organizing Latino Power and Action, or COPAL, is a member-based organization working to improve the quality of life for Minnesota Latine communities since 2018. Cecilia Calabria is COPAL’s Health and Wellness Director.
“We are beginning to break down the barriers Latines face when accessing health care.” - Cecilia Calabria, Health and Wellness Director, COPAL
COPAL connects families to essential services when they need them most.
“During the onset of the COVID-19 pandemic, COPAL launched the Navigator’s Hotline because community members were reaching out to COPAL to get help with a variety of issues,” said Calabria. “Our navigators connected people with food resources, testing sites, contact tracing, public benefits, health care, housing assistance, and more.”
The navigators also partnered with churches, schools, and Latino markets to spread information, communicate with community members, and provide disease prevention education.
COPAL hosted a community conversation to learn about the issues families faced due to the pandemic. One pressing need was accurate health information in Spanish.
This need led to the Promotoras de Salud, or Health Community Educators’ program. COPAL trained staff and recruited the first cohort of promotoras de salud from the Twin Cities, Mankato, and Rochester areas in 2022. By early 2023, the first group graduated with the skills and knowledge to discuss sensitive health topics and foster productive conversations. Promotoras de salud will continue to play a critical role in bringing preventive health education to Latine communities.
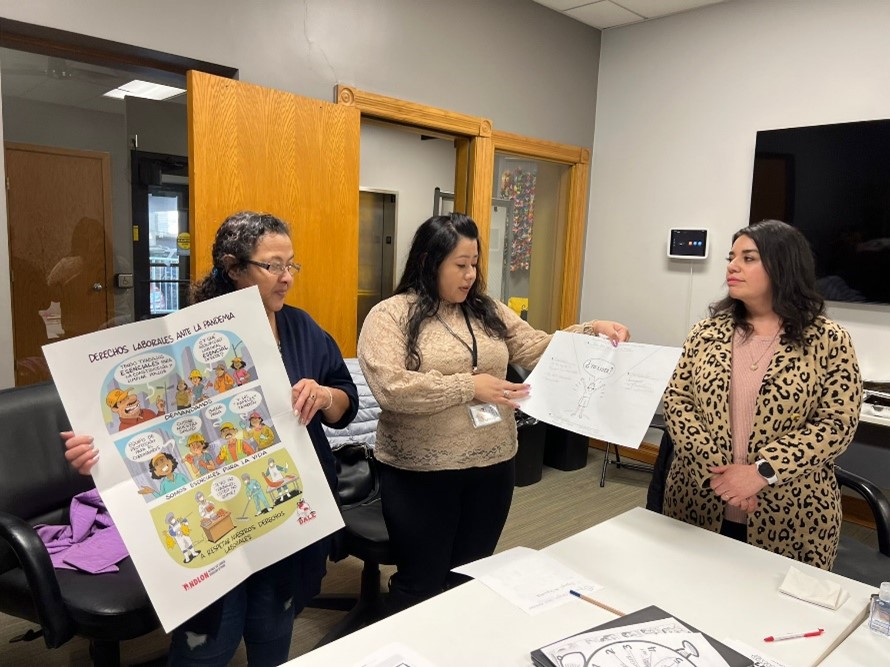
The goals and work of COPAL go on. Calabria said she hopes to train a second cohort of promotoras de salud and expand the program to bring more Latine people into the health care industry. COPAL also plans to create new and deeper partnerships with service providers.
“COPAL envisions a future where Latine communities thrive and are fully empowered to lead significant change in their communities and beyond.” – Cecilia Calabria
Connecting to meet mental, physical, and emotional needs | August Health Equity Networks Newsletter
View the full August newsletter: MN Health Equity Networks Aug 2023 Newsletter
Mac Reed was raised in Mora, Minnesota by their grandparents, and from their grandparents learned about community and neighbors helping neighbors. “My grandparents taught me that if you see a need, then fill the need,” says Mac, who uses they/them pronouns. Mac’s grandparents influenced them to carry on their family’s tradition of community involvement.

Mac Reed, Technical Services Assistant at East Central Regional Library
As a librarian at the Mora Public Library (a branch of the East Central Regional Library) at the time of the COVID-19 pandemic, Mac saw the library was a trusted community resource for information and services. “Libraries are so ingrained in our communities. We sometimes were the only people that folks talked with each week,” says Mac.
Mac saw that the library became a key source of information in their community: “[People would] hear something on TV or on the radio, maybe a comment from a friend, and they’d call us, asking, ‘Is this right?’” says Mac. “They looked to us for help and answers, and we did our best.” Finding answers often required deeper research. “We’d call up Welia Health and tell them we needed information,” says Mac, of the health system with a clinic in Mora. “We’d get current and accurate details for our patrons. We’re librarians and we know how to collect and distribute data.”
Connecting people to information proved another challenge. “We started hooking people up to the internet. Before COVID, our library system had a total of 30 hot spots our patrons could check out,” Mac says, of the hardware that enables users to connect their computers or mobile devices to Wi-Fi. “We quickly realized that we needed to get more. Those hot spots were an important way for us to help people connect during COVID.”
“In a way, we were a lighthouse in the middle of COVID.” – Mac Reed, East Central Regional Library
That began driving what Mac calls a “subtle curve” in the direction in which the library helped their patrons, in addition to offering traditional library services. Prior to the pandemic, the library offered free snacks in the teen section. During the height of the pandemic, the snack bin grew to provide snacks for all library patrons, with a collection of easy-to-eat or easy-to-make foods in an inconspicuous spot in the library.
Soon the library started collaborating with a local food shelf to offer even more. “A food shelf volunteer came over, took measurements of an unused coat closet, and built us shelves that fit perfectly,” says Mac. “The food shelf folks brought the food over, and the library staff took care of it.” The library and the food shelf signed a formal contract, and the library food shelf became an important source of emergency food, since the library’s daily hours extended beyond those of the food shelf. In addition, patrons needing food weren’t required to share their names or identification at the library. Mac shares patrons would ask: “So, it’s just free?”

Mora Public Library’s on-site food shelf
Library staff noticed other unmet needs, and community members donated funds for diapers, period products, soap, deodorant, other foodstuffs, and more. Signs in bathrooms hold tags showing a variety of diaper sizes; patrons can grab a tag, bring it to the desk, and staff discretely give them diapers. After the Supreme Court overturned Roe v. Wade in June 2023, the library reached out to local clinics for information on birth control and other resources, and now distributes free pregnancy tests upon request.
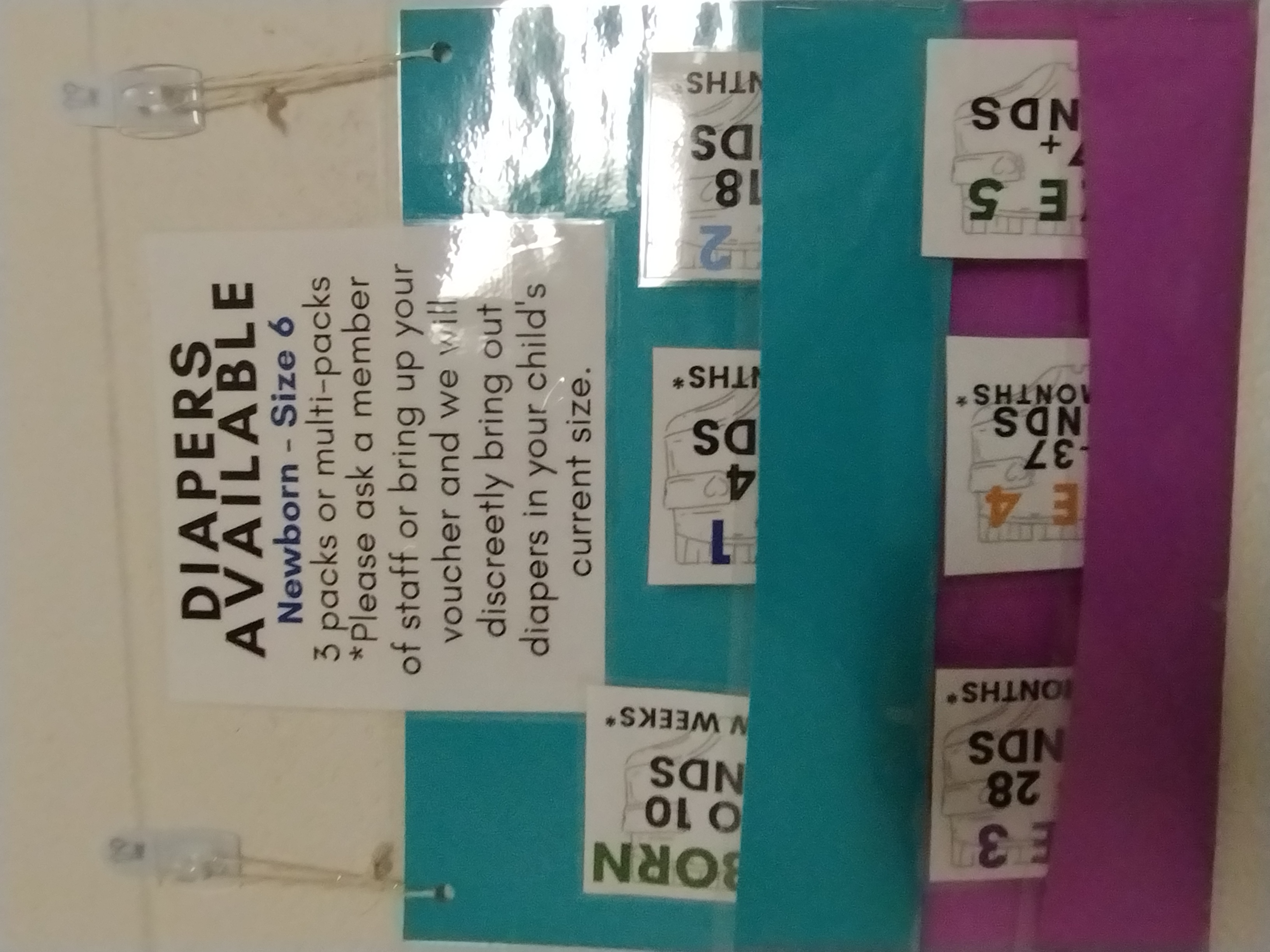
Diaper tags are available for patrons to exchange for diapers
Mac thinks of the library as a microcosm of their community, and working there gives them a unique glimpse into it. “We get a layered image, a multi-level snapshot here. We see situations from every angle, and gather information to make a whole picture,” they say.
“At the end of the day, every library works toward health equity in their own way.” – Mac Reed
The library’s work has not gone unnoticed. In October 2022, the Mora Library was awarded Lakes and Pines Community Action Council’s Spirit of Community Award. The library also collaborates with local Master Gardeners, library volunteers, and other community organizations.
In the future, the library hopes to offer more support for sustainable living.
Mac Reed, Technical Services Assistant for the East Central Regional Library System, will present information about their revolving seed library at the Minnesota Library Association Child and Young People’s Unconference, on September 8, 2023.
Laying the groundwork for equity with a Health Equity Advisory and Leadership Council: Network member spotlight with Rice County HEAL Council
View the full July 2023 newsletter:July 2023 Health Equity Networks Newsletter

"This work is just starting and the journey is the goal." - Sara Coulter, Rice County Public Health Clinic and Community Supervisor
Sara Coulter has been working on the creation of the Rice County Health Equity Advisory and Leadership (HEAL) Council since last year, when the county was awarded a grant from the Minnesota Health Equity Network. She and other staff are connecting with community members and organizations, inviting them to join the council, and asking them how they think participation should look. They are starting by talking to the people with whom they have solid relationships and mutual trust. They hope to get input from them about possible new contacts, locations for meetings that are most comfortable for community members, what size of group might feel right to them, what communication needs they should address, and details on other barriers to participation.
"COVID was the quick work. This is an engagement. It’s the slow work of sitting down and listening. We plan to take our time and build trust." - Sara Coulter
Throughout the COVID response, Rice County Public Health staff worked with community groups and diverse media on education and messaging. The HEAL Council aims to build on those existing relationships and connections, and gain a better understanding of the community’s vision of health. "We know that we have much to learn," says Sara. "Above all, we want to know how the HEAL Council can serve as a true source of the work of healing our community."
One of the HEAL Council's goals of is to make sure that community members feel they can freely express their needs and ideas, and therefore completely participate. Interpreters will be plentiful, to make communication as easy as possible.

In addition, Sara welcomes contact from other organizations working toward health equity, to share information, questions, and experiences. "Susan Brace-Adkins from [the Minnesota Department of Health] calls the people doing the same kind of work as we do 'near peers.' I really like that phrase and have always benefitted from collaborations with near peers," says Sara. "I welcome the contact with others who may have ideas or questions about the HEAL Council. Reach out; send me an email. Let’s build a relationship."
"We hope that at some point in our time together people will mix in new ways and leave meetings feeling as though they are part of the action that will create change for themselves and their communities." - Rice County HEAL Council proposal
Read more about the Rice County HEAL Council: Faribault Diversity Coalition series highlights health equity (Faribault Daily News)
Building on relationships: Network member spotlight with Wright County Health Equity Learning Squads
View the full June newsletter:June 2023 Health Equity Networks Newsletter

"We start with relationships with the people we see day to day, and build on them to make things happen." - Ellie Vanasse, Wright County Public Health Nurse and Health Equity Action Team (HEAT) Organizer
Wright County Public Health Nurse Ellie Vanasse helped start the county's Health Equity Action Team (HEAT) about four years ago. They have organized a number of health equity projects in that time, but the effort with the most impact is the Health Equity Learning Squads project. The squads are micro-discussion groups who meet monthly to reflect on and learn about the way they do the work of health equity.
Squad members begin by reading articles, watching videos, and discussing issues such as identity, as that offers more opportunity for connection. HEAT encourages a focus on a number of values: relationship and connection, practice not perfection, curiosity, realness, collectivism, and strategic and thoughtful risk-taking. According to Ellie, "They can talk about hard things, and don’t just take no for an answer.” Squad members offer each other support and understanding, strengthen their relationships, and experience personal and professional growth. Annually, all of the squads gather for a Squad Summit.
"Employees have resigned or retired, but no one who has joined has dropped out of a squad. People show up because they want to show up, and I’m extremely proud of the fact that they do." - Ellie Vanasse
In the beginning, fifteen people joined Health Equity Learning Squads. Since then, staff participation has increased. There are now seven squads in the department, each made up of three to five people. Squads meet approximately once a month, and sessions last about an hour with another hour of work done between meetings. They have the option of meeting more often if they choose, but never more than once a week. All the squads also gather annually for "squad summits."
The small size of the squads were an intentional choice. Scheduling meetings for smaller groups is less complicated. But more than that, keeping the squads small offers people more time to talk, to build relationships, and have deeper discussions.
When you are in a group of three, your voice is heard. Just because there are less people at the table doesn’t mean they are less involved. - Ellie Vanasse
HEAT also offers monthly opportunities to all Wright County Public Health employees, including training on topics such as name- and identity-sharing, information on social determinants of health, opportunities to participate in book clubs and podcast discussions, in-house newsletters, and surveys regarding staff understanding of health equity work. Management does not participate in the squads, but members of management attend HEAT-sponsored workshops and trainings and are considering creating their own squads.
It all started when in 2019 Wright County staff participated in a climate justice project through the Human Impact Partners Initiative. Six of them decided to use what they learned in the project to address health equity within the Wright County Public Health Department. They liked the Human Impact Partners project model, which includes discussion and a dive into personal and professional perspectives, so used it to draft a plan. They presented the idea of Health Equity Learning Squads to the Wright County Public Health Director, Sarah Grosshuesch, who approved and supported the project. Any staff who was interested, regardless of their position, could join a Health Equity Learning Squad. She also communicated her support throughout the department, and announced that time spent preparing for a squad meeting or attending one would be considered work time. Ellie says, "We came up with the ask and management was super supportive."

Three-quarters of all Wright County Public Health staff now are members of a squad. The original HEAT members are part of the squads, and continue to check with and support other squads. At last year’s MPHA, the HEAT presented information on their project. The team is drafting a squad guide in order to document the experience. They also recognize the gaps in their workforce and are working to encourage more diversity. Above all, according to Ellie, they are aware of the "extreme privilege" they have in "getting paid to talk about health equity."
"The goal is to deepen relationships, disrupt master narratives, answer the question of how to make meaning in the world and transform ourselves and our work toward equity." - Health Equity Learning Squads; Human Impact Partners model, draft document
Want to learn more about the Health Equity Learning Squads? Ben Grimm from Wright County Public Health will present at the Central Regional Health Equity Gathering on July 26, 2023. Register and join us!
The Intersection of Data and Equity: Network member spotlight with Carlton-Cook-Lake-St. Louis Community Health Board
View the full May 2023 newsletter: May Health Equity Networks Newsletter
Members and staff of the Carlton-Cook-Lake-St. Louis Community Health Board wanted to know more about how to build more equity into data systems and make more data-informed decisions. The community health board applied for and was awarded a Regional Health Equity Networks grant to use to provide this training. Stephany Medina, the Program Manager and Public Health Planner for the community health board, remembered attending an excellent data equity training by an organization named We All Count while working for a member of the Feeding America network.
"It was important to learn together so we were coming from a place of shared language and understanding of data equity." - Stephany Medina, Carlton-Cook-Lake-St. Louis Community Health Board
Community health board staff got together with Heather Krause from We All Count to plan and offer two-part virtual training, called "Foundations of Data Equity." It was customized for people who were not experienced data analysts and emphasized a community perspective. Representatives from local public health, nonprofits, academic institutions, public schools, the Minnesota Department of Health, and others attended the training, which was held in early April 2023.
"The folks from the Carlton-Cook-Lake-St. Louis Community (Health Board) training asked some really fabulous questions that are directly related to the importance of making thoughtful, equity-informed choices for the unique needs of projects rather than try to develop some type of across-the-board checklist of best practices. They’re well set up for small, sustainable steps – which is the ideal (in order) to find success in equity and data projects." - Heather Krause, Founder, We All Count
Data-informed decision-making is becoming a bigger priority for many health departments and related organizations, as they learn from COVID-19 response and adapt to future challenges. "Data-informed decision making" means that organizations use numbers to guide decisions and, due to this, have more confidence that they are making the right choices. Numbers are the tools used to plan programs, evaluate initiatives, or create improvement strategies. But inequitable data can also lead to inequitable decision-making.
"The first thing that was highlighted in the training is the fact that data isn’t objective. As much as we’d like to believe that we use objective processes to gather and analyze data, and that if we use that data just right, we can come to objective and conclusive answers; that isn’t reality." - Stephany Medina, Carlton-Cook-Lake-St. Louis Community Health Board
Organizations and people make subjective decisions at every step of data projects from motivation to data collection, from analysis to interpretation, and even how to use and share results. Organizations and people make decisions about who to center in every data project (e.g., students, teachers, or researchers). Organizations and people also make decisions about which results to consider significant, and which results are not significant. The training addressed the question, "If objective data doesn’t exist, what does that mean for equity goals?"
During the training, We All Count made some basic recommendations:
- Be clear about equity goals.
- Decide who to center in your project.
- Determine the learning goal.
- Find out if all partners (program participants, funders, program coordinators) want to learn the same things.
- Be intentional.
- If you wish to center program participants, design your evaluation or data project to center the goals and perspective of program participants.
- Be transparent.
- Communicate the choices made and the reasons you made those choices in your results.
Heather also shared the data equity framework below, outlining a systematic way of looking at data projects. It organizes every project into seven stages:

Above all, the data equity training offered people the opportunity to learn about how to craft more equitable data plans and design clear, intentional, and transparent programming.
"Since taking this training a week ago, I haven't stopped thinking about it. It totally reframed how I think about equity and data. And, as a non-data scientist, I found it very approachable and relatable to my work, which was an exciting surprise!" - Foundations of Data Equity training participant
Carlton-Cook-Lake-St. Louis organizers were pleased with the success of the training and with attendee responses.
"We All Count shared a wealth of knowledge during the Foundations of Data Equity training. While we know this training doesn’t mean all our data-informed decision making efforts are now equitable, we hope this brings us one step closer to embedding more equity into the work that we do." - Stephany Medina, Carlton-Cook-Lake-St. Louis Community Health Board
Image credit: We All Count
Community means connection: Network member spotlight with Growing Up Healthy
View the full April 2023 newsletter: April Health Equity Networks Newsletter
In many ways, Fatima Ponciano grew up alongside Growing Up Healthy. In 2006, as a high school student, she started volunteering with Growing Up Healthy as a community representative. Now, as an Early Childhood Navigator with the organization, she says, “It’s been interesting and wonderful to see it grow.
Growing Up Healthy works with partner organizations and Latine and immigrant families in Faribault and Northfield to transform communities by cultivating neighborhood leadership, fostering social connectedness, and collectively advocating for systems-level change.
That connectedness is key, says Fatima. “When we started, we held community meetings to hear from people about the challenges and issues they were experiencing,” she says. “One of the things that we kept hearing was that people felt disconnected from the community and resources and also disconnected from each other.” The organization hopes to continue expanding in Rice County, supported by the Healthy Community Initiative, its parent organization.

“We want this to be a place where no one has to worry about the forecast or whether their furnace is working,” says Fatima, “where everyone can afford childcare, preschool, or day care, [and] above all, where everyone has a safe place to live.”
Growing Up Healthy works with partners to help fill some of these gaps by:
- Connecting residents in Faribault and Northfield mobile home parks with home energy improvement programs; organizing a Heat Tape Outreach program; partnering with Xcel Energy to organize Home Energy Squad visits
- Helping parents and caregivers develop leadership skills and organize to positively change systems to benefit children in their communities
- Organizing community events to deepen social connections and promote neighborhood outreach
- Working with Faribault and Northfield expectant parents and families with young children to connect them with early learning and kindergarten preparation, in partnership with WIC, HealthFinders, Rice County Public Health, Allina Partners, and others
- Providing free home visiting services in Rice County to a number of children, thanks to a partnership with Jewish Family and Children’s Services and Parent Child Plus; promoting learning through play, enhanced parenting skills and school readiness
- Supporting families and childcare providers navigating Child Care Assistance
- Improving elementary school students’ attendance and engagement by working with students and their caregivers to promote success in schools
- Distributing breakfasts, lunches, and weekend meals during the pandemic, funded through a grant collaboration with No Kid Hungry, Faribault Public Schools, and Growing Up Healthy

“There are barriers and obstacles that we are unable to tackle, but that’s where our partners and referrals come in,” says Fatima. “Luckily, we have strong connections, and we’ve learned to get all our community organizations involved. Thanks to those collaborations, we’ve seen some systems-level changes.”
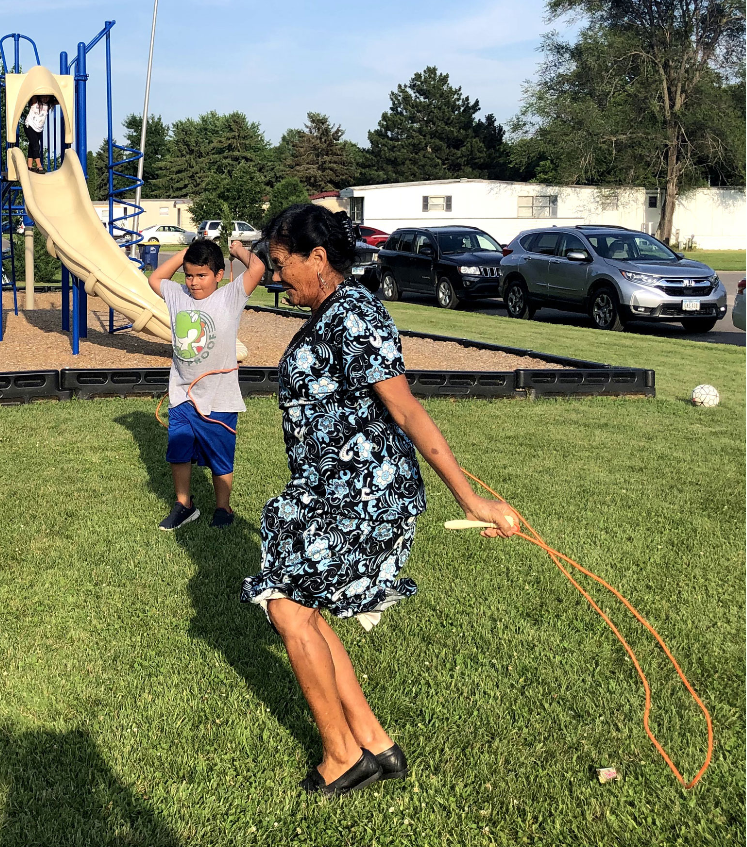
Photo credit: Growing Up Healthy
Connecting people to the care they need leads to "best possible outcomes": Network member spotlight with HealtheMed
View the full March 2023 newsletter: March Health Equity Networks Newsletter
Avery Kennett understands the challenges often faced by Minnesotans using Medicaid waivers. As enrollment manager at HealtheMed, she is part of a team that helps people overcome health care access barriers by connecting them with medical services right in their homes. “Being able to monitor and share client data and medication information with their doctors helps clients remain happier and healthier,” says Avery.

“We work to reduce not only the stress on the client, but also on the county and the health care system,” says Avery. HealtheMed offers remote-patient monitoring with a variety of devices including automated medication dispensers, contactless thermometers, pulse oximeters, blood pressure cuffs and weight scales. All are connected through a 50-inch Smart TV installed in the clients’ home. Physician visits occur on the Smart TV rather than a cell phone—which makes the experience more immediate and effective. Clients can access health information, educational videos, and other services via the Smart TV.
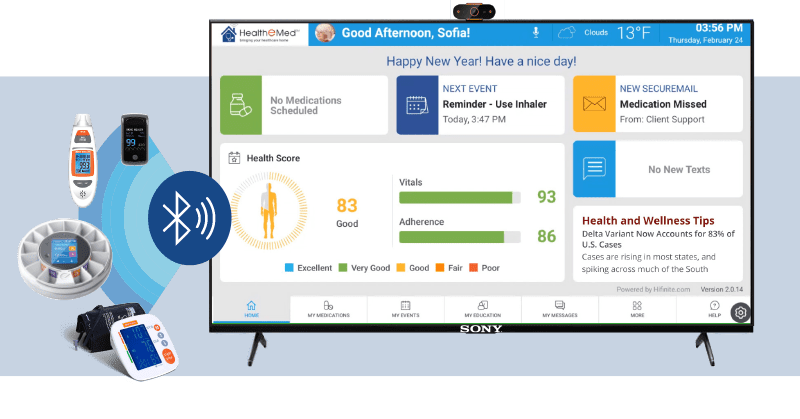
But HealtheMed doesn’t just rely on technology to close the access gap for its clients: HealtheMed collaborates with providers to deliver mental health and pharmacy services. Skilled nurse consultants meet in person with clients quarterly, and regularly connect the clients to their practitioners. Avery adds, “The nurse consultants can really help guide and educate. They add a layer of support and a safety net.”
“We have been able to bring health care access into our clients’ homes, which has been super powerful, and has increased their quality of life. We want them to have the best possible outcomes,” she says.
Four founders developed HealtheMed five years ago, working with the Minnesota Department of Administration to find creative solutions for reducing the cost of care and bridging service gaps. “We started by becoming a Home and Community Based Provider,” says Avery. “Then we found doctors and behavioral health specialists who were very motivated to serve Medicaid enrollees with waivers. That was our genesis.” HealtheMed refined its business plan and launched in September of 2020, exactly when telemedicine technology was sorely needed during the height of the COVID-19 pandemic. Currently, the organization serves 200 clients in 22 counties.
One problem HealtheMed staff tackle is medication non-adherence: “Our clients have achieved an overall medication adherence rate of 79 percent so far,” says Avery, emphasizing the successful results that have been achieved.

Remote patient monitoring also helps families when health care settings are stressful: “One of our clients has three children, all of whom are on the autism spectrum, and are on three different medication regimens. One child was so stressed before doctor appointments that it was necessary to medicate them. The remote patient monitoring eliminated a lot of barriers for the family. The mother was able to track the medication management far more easily. Above all, it resulted in less stress for everyone, especially for the kids.”
Another client, a double transplant recipient who is also receiving mental health care, found it overwhelming to track and manage his health issues. He worked with HealtheMed’s team, who helped him successfully set up and use remote patient monitoring. “He gets reminders to step on the scale, take his vitals, and it stores the data for him,” says Avery. “Now he feels empowered because he can help navigate his own health.”
HealtheMed is constantly evolving and plans to continue to expand its footprint in Minnesota. “The more we learn about our clients,” Avery says, “the more we can expand and keep people in their homes and out of the hospital.”
“Not many organizations are doing both service and technology. We have the capability to be individualized, and that sets us apart,” says Avery. “Above all, we know that the human touch is essential and that every one of our clients has a different story to tell.”
Join your regional Health Equity Network and find ways to partner organizations like HealtheMed, to connect, strengthen, and amplify health equity in your region!
Photo credit: HealtheMed, Adobe Stock
Trust and collaboration help build healthy families: Network member spotlight with First Steps to Healthy Families
View the full February 2023 newsletter: February Health Equity Networks Newsletter
Kami Kelm understands the fear some families feel when they interact with county social services or other government programs. She sees it in her work as case manager for First Steps to Healthy Families in Beltrami County: "One of my biggest challenges is just to get people to answer the door or the phone." But she also knows that the power of connection. When a community supports a family, that family can more easily get what it needs. "When I can connect and we can talk honestly, we have had some amazing turnarounds," she says.

Eight years ago, Beltrami County started First Steps to Healthy Babies, in partnership with the Red Lake Nation, Sanford Health, and others, to help parents with prenatal care and sober supports. It provided postpartum services until a baby turned one year old. Today, that program has expanded to operate as First Steps to Healthy Families, and Kami works with families until children turn five years old.
"We really have to work together to meet the needs of our community. We have to do a lot with less, and that requires relationships." – Jeff Lind, division director, Beltrami County Social Services
Above all, First Steps to Healthy Families seeks to help participating families understand that pregnancy is not a cure for addiction. Their model has expanded to other counties and communities, and the team networks with similar programs to compare notes. "We were the guinea pigs. To see it now is really cool," says Kami.
Jeff looks at the big picture, and thinks a county made up of rural and small-town residents has the strength of community and collaboration on its side. "We certainly have all the challenges you’d see in urban areas,” says Jeff. “Our rates of overdose and deaths from overdose are very high. But what we do have in our county is [our] collaborative nature. We don’t have the resources that other more urban areas do, so we really have to work together to meet the needs of our community. We have to do a lot with less, and that requires relationships."
"There’s not always a quick answer for every person, but within the community we can piecemeal things together. That’s what happens when you do enough collaboration. It is those connections that lead me to opportunities to help someone." – Kami Kelm, case manager, First Steps to Healthy Families
Kami recalls helping a mom of four living in unstable housing. Without any means of transportation, the family couldn’t connect with the services they needed on their own, so Kami drove them to the Red Lake Nation government office for the day, where the children were enrolled as members and they could get on a tribal housing waitlist. "We just took a day, drove over, and got it all done," explains Kami.

Kami and Jeff explain that First Steps to Healthy Families has evolved and changed through the years, as grant funding comes and goes, resources ebb and flow—not to mention COVID, which "threw a curveball, and changed partnerships and routines," says Kami.
People also use different substances than they did when First Steps first started. Substance use has moved from opioids to heroin and meth to fentanyl. "People are getting stronger and stronger drugs," says Kami. "We have to be aware of the trends and also the resources available. When we see something new, we all share information with each other."
Jeff and Kami have also seen advances in approaches to substance use such as an emphasis on harm reduction and medically assisted treatment, which means First Steps to Healthy Families has more options to help support the families in the program. "The freedom that we have to tailor this project to the community is really cool," says Kami.
"Every community should have something like this and work with families, not against them." – Jeff Lind, division director, Beltrami County Social Services
Read more about how First Steps to Healthy Families helps families get the help they need:
- Epidemic led to dramatic rise in foster care cases, emergency calls (Bemidji Pioneer, 2022)
- First Steps to Healthy Babies: Program aims to reduce opioid-affected births at rural hospitals (MinnPost, 2018)
- Sanford Bemidji’s First Steps program helps addicted mothers, babies (Bemidji Pioneer, 2017)
- A heart-breaking consequence of the opioid crisis: Addicted babies (Minnesota Public Radio, 2017)
Join the Northwest Health Equity Network and find ways to partner with First Steps to Healthy Families and other organizations to connect, strengthen, and amplify health equity in your region!
Photo credit: Adobe Stock
"Every community should have something like this and work with families, not against them." – Jeff Lind, division director, Beltrami County Social Services
Read more about how First Steps to Healthy Families helps families get the help they need:
- Epidemic led to dramatic rise in foster care cases, emergency calls (Bemidji Pioneer, 2022)
- First Steps to Healthy Babies: Program aims to reduce opioid-affected births at rural hospitals (MinnPost, 2018)
- Sanford Bemidji’s First Steps program helps addicted mothers, babies (Bemidji Pioneer, 2017)
- A heart-breaking consequence of the opioid crisis: Addicted babies (Minnesota Public Radio, 2017)
Join the Northwest Health Equity Network and find ways to partner with First Steps to Healthy Families and other organizations to connect, strengthen, and amplify health equity in your region!
Photo credit: Adobe Stock
It's all about relationships: Network member spotlight with Dakota Child and Family Clinic
View the full January 2023 newsletter: January Health Equity Networks Newsletter
Metro Health Equity Network member organization Dakota Child and Family Clinic turned 10 years old last year. After facing closure in 2011, the community around the clinic organized, formed a board, and applied for nonprofit status. Community members even personally painted and improved the clinic building, living out their mission: Providing health care for people, not for profit.

Kelly Kenley, Executive Director, shares the the clinic's "whole person, whole picture" focus, and notes its emphasis on a nurse practitioner model. Clinic highlights include:
- After meeting with staff, it is discovered that a patient suffering from back pain is also homeless. Some of the problems are because the patient is sleeping on floors and couches. The clinic works to help the patient find a comfortable place to sleep.
- A child with medical trauma isn’t able to be inside the clinic for a visit. The clinic staff walks out to the family car in the parking lot and examines the child there.
- Another patient has high blood pressure, apparently related to stress. The clinic assists with medications, but they also support the patient by helping them access mental health services.
- A family new to the country brings a child into the clinic who is suffering from severe abdominal pain. It becomes clear that they need to go to the hospital. The family has applied for insurance, but it is still in process, so affordable transportation options are limited. The staff arranges and personally pays for Lyft transportation to get them to the hospital.
- The clinic provides free initial health care appointments at Mission Outpost, a local food and resource center, with a sliding fee scale for continued care if needed.
- Services for Spanish-speaking and Russian populations are available, and some staff have completed a medical translation program to assist in case management.

The clinic also offers mental health services. Kenley relays the clinic's struggle, "We aren’t going to one-to-one our way out of the current mental health crisis. So what other things can we do to support mental health?" The clinic organizes support groups under headings like "It’s Complicated" and "Safety Net," alongside Spanish-speaking support groups, support groups for families with challenging children, and a local Transforming Families chapter. A social worker attends many of these meetings, connecting participants to services and follow-up. "When something is hard, it helps when somebody knows you’re struggling," says Kenley.

Kenley also notes COVID has been the impetus for significant growth. "It offered a unique opportunity we would not have had otherwise," she says. The clinic offered barrier-free COVID testing and drive-up testing in three locations in Dakota County, with no ID required. The clinic also offered on-site testing at three local school districts during the 2020-2021 school year. By advocating with Dakota County, the clinic could reduce barriers and wait times.

And in the future? Dakota Child and Family Clinic's hope is to expand to other food shelves and shelters. Staff dream of outfitting a mobile unit. According to Kenley, "Our efforts raised our profile in the community. We built more trust, and it’s a privilege to have earned that. Now that we have, there is so much to do. It can be overwhelming at times. But it’s all about relationships."
To learn more about Dakota Child and Family Clinic, join us at the January 24 Metro Region Health Equity Network gathering for the region's member spotlight.
Join the Metro Health Equity Network and find ways to partner with Dakota Child and Family Clinic and other organizations to connect, strengthen, and amplify health equity in your region!
Photo credit: Dakota Child and Family Clinic
2022
We're building health equity together!
View the full November newsletter: November Minnesota Health Equity Networks Newsletter
Inaugural newsletter from the Minnesota Health Equity Networks
View the full October newsletter: Welcome to the inaugural Health Equity Networks newsletter!
Connect: Who should join their Health Equity Network?
A note from Shor Salkas, project supervisor ...

Relationships are a core human need. We need to know the people that are our neighbors, that we work with, that live in our communities. The people around us lift us up and support us in our struggles. We thrive as individuals and as communities when we are connected.
And this applies to our work in public health and advancing health equity, as well. A relational approach to changing our world is not new, but it is still revolutionary. We are asking you to show up, get curious about each other, and deeply care about each other and about changing our communities and systems to ones that heal, not harm.
 We invite you to regional network gatherings and connect to each other in intentional ways—to get curious about how to lift up your successes and collaborate on how to go deeper in supporting your communities. The networks will also offering trainings and coaching throughout the year to deepen knowledge on a variety of health equity issues that are important to communities across the state. All of our offerings are open to your thoughts and feedback, because mostly, we want to get to know you.
We invite you to regional network gatherings and connect to each other in intentional ways—to get curious about how to lift up your successes and collaborate on how to go deeper in supporting your communities. The networks will also offering trainings and coaching throughout the year to deepen knowledge on a variety of health equity issues that are important to communities across the state. All of our offerings are open to your thoughts and feedback, because mostly, we want to get to know you.
To find the coordinators, dates of gatherings and trainings, check out our website at Minnesota Health Equity Networks and click on "Events and training opportunities."
Who belongs in the Minnesota Health Equity Networks?
The short answer is anyone. One of the goals of this project is to support the public health system and to come together around health equity and community engagement issues in new and different ways. So expect a lot of folks from "the public health system" in network gatherings and spaces. But network staff have also been building relationships with community organizations, folks in Tribal health, and throughout our regional communities.
Come as you are, and we invite you to come:
- With an open mind and open heart
- With curiosity
- Ready to get comfortable with discomfort
- Ready to meet and connect with people, new and familiar
- As a life-long learner
There are no membership criteria. We hope that you will join us and together we can connect our communities, strengthen our work, and amplify our achievements. Together we can work toward promoting health equity in Minnesota.
Read the rest of the October 2022 newsletter at: Welcome to the inaugural Health Equity Networks newsletter!
Funding for this project is provided by the CDC OT21-2103 COVID-19 Health Equity Grant.