Enhancing workflows and improving care
At each visit, every patient completes the wellbeing screener with the option to opt out. Southside Community Health Services also uses the PHQ-9, a validated tool that assesses depression symptoms. They also ask patients questions from the GAD-7 regarding anxiety and a modified PRAPARE tool to learn more about social determinants of health that may impact the patient.
Learn more about the screening tools:
If a patient indicates they may be at risk for depression, they get connected to a therapist or other behavioral health resources as needed in the clinic. Through the new process, therapists are available for consult on each shift and staff work to ensure patients feel safe and comfortable.
If patients need more advanced services, the clinic refers them to outpatient care, community support programs, and more. They also provide more care coordination and help patients with scheduling appointments, transportation, and what they need to better manage their health.
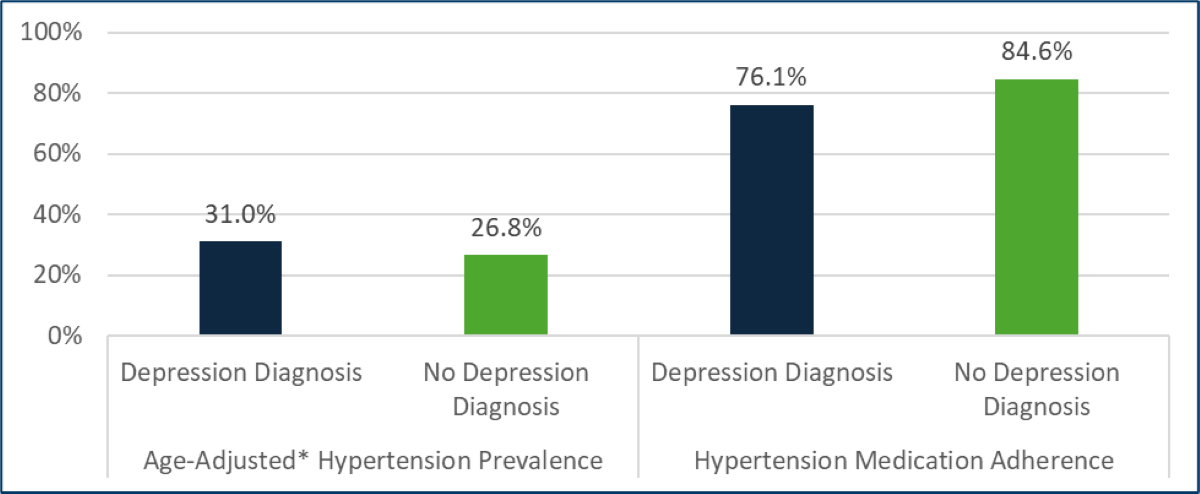
Because of the coordinated screening for both health-related social needs and mental health, care providers at Southside Community Health Services gain a more comprehensive picture of their patients’ health and develop care plans that are better tailored to meet the needs of those who have been diagnosed with hypertension and/or depression.
The workflow model that Southside developed not only has significantly improved how the clinic supports patients, but it can also be replicated for other initiatives and in other clinics.
Screening rates in the clinic have drastically improved: depression screening went from 70% to around 90% and screening for social determinants of health went from 2% to 18.6% over the course of a year.