Contact Info
Syphilis: Aid to Diagnosis
On this web page, you will see some extremely graphic images. These images are intended to help health care professionals identify and diagnose syphilis. We do not suggest proceeding unless you are a health care professional who needs to see such images. Thank you.
All images and descriptions courtesy of the CDC Public Health Image Library
- Download this page formatted for print: Syphilis: Aid to Diagnosis (PDF)
On this page:
Primary
Secondary
Tertiary/Late Stage
Primary:
Usually, a single ulcer (chancre) appears at the site where the bacteria entered the body. The genitals are the most common location for chancres to develop, but these ulcers also can form around the mouth or anus. The chancre is firm and painless, and it oozes fluid that contains syphilis bacteria. Sometimes, lymph nodes near the ulcer become enlarged, but remain painless. The chancre of primary syphilis usually heals after one to five weeks, although the person remains infected. At this stage, syphilis is highly contagious.
- Painless lesion appears 10-90 days at site of exposure, persists for 1-5 weeks
- Multiple lesions (25% of patients)
- Often goes unnoticed if it’s not someplace obvious, i.e. inter-vaginally, rectally, orally
Primary syphilitic chancres
Primary syphilitic chancres are usually firm, round, small, and painless, and develop at the spot where the T. pallidum bacteria enter the body. The chancre lasts 1 to 5 weeks, and it heals without treatment. However, if adequate treatment is not administered, the infection progresses to the secondary stage.

This patient presented with a penile chancre located on the proximal penile shaft, which was diagnosed as a primary syphilitic infection.
Photo Credit: CDC/ Dr. N. J. Fiumara; Dr. Gavin Hart

This patient presented with a penile chancre located on the proximal penile shaft, which was diagnosed as a primary syphilitic infection.
Photo Credit: CDC/ Dr. Gavin Hart; Dr. N. J. Fiumara

This image shows chancres on the penile shaft due to a primary syphilitic infection.
Photo Credit: CDC/M. Rein, VD

This patient presented with a primary vulvar syphilitic chancre.
Photo Credit: CDC

A patient with a primary syphilitic vulvar chancre, and condyloma acuminatum, or genital warts.
Photo Credit: CDC/ Susan Lindsley

This patient presented with a primary anorectal syphilitic chancre during the primary stage of the disease.
Photo Credit: CDC/ Susan Lindsley, VD

This patient presented with an anal chancre due to Treponema pallidum bacteria.
Photo Credit: CDC
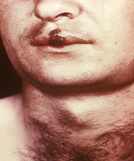
This patient presented with a primary syphilitic chancre of the lip.
Photo Credit: CDC

This patient presented with an extragenital facial chancre of the lip.
Photo Credit: CDC
Secondary:
Secondary syphilis is characterized by a systemic spread of the Treponema pallidum bacterial spirochetes. Skin rash and malaise commonly characterize the secondary stage. The signs and symptoms of secondary syphilis will resolve with or without treatment, but without treatment, the infection will progress to the latent and late stages of disease. At this stage, syphilis is highly contagious.
- “Rash” 75%-90% of patients
- Malaise, fever 50-80%
- Mucous patches oral cavity and genital areas 5-30%
- Moist, heaped, wart-like lesions — Condyloma lata — on genital, anal or oral areas 5-25%
- Hair loss 10-15%
- Neurosyphilis <2%
Characteristic rash
The characteristic rash of secondary syphilis may appear as rough, red, or reddish brown spots both on the palms of the hands and the bottoms of the feet. However, rashes with a different appearance may occur on other parts of the body, sometimes resembling rashes caused by other diseases. Sometimes rashes associated with secondary syphilis are so faint that they are not noticed.

This patient presented with secondary syphilytic lesions on the palms of her hands.
Photo Credit: CDC

Close-up view of keratotic lesions on the palms of this patient’s hands due to a secondary syphilitic infection. Photo Credit: CDC

This patient presented with secondary syphilytic lesions on the palms.
Photo Credit: CDC/ Susan Lindsley

This patient presented with secondary syphilitic lesions on the plantar aspect of the foot.
Photo Credit: CDC/ Susan Lindsley

This patient presented with secondary papular syphilids on the soles of his feet.
Photo Credit: CDC/ Susan Lindsley

This syphilis patient presented with a “roseola rash”, similar to that of viral eczema, which developed on her buttocks and legs during the secondary stage of the disease.
Photo Credit: CDC/J. Pledger, BSS/VD

A photograph of a secondary syphilitic papulosquamous rash seen on the torso and upper body. Photo Credit: CDC/ Susan Lindsley

This patient presented with a secondary syphilitic rash covering his back.
Photo Credit: CDC / Dr. Gavin Hart

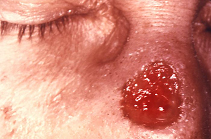
The pustules shown under this patient’s chin are due to a secondary syphilitic infection.
Photo Credit: CDC
Mucous patches
Mucous patches form during the breakdown of mucous membranes, seen here on the inferior surface of the tongue. During the secondary stage of syphilis, mucous patches can also develop inside the mouth, vulva, and vagina.

A photograph of mucous patches on the tongue due to secondary syphilis.
Photo Credit: CDC/ Susan Lindsley

This image depicts a lingual mucous patch on the tongue of a patient who was subsequently diagnosed with secondary syphilis.
Photo Credit: CDC/ Susan Lindsley
Tertiary/Late stages:
Without treatment, an infected person still has syphilis even though there are no signs or symptoms. It remains in the body, and it may begin to damage the internal organs, including the brain, nerves, eyes, heart, blood vessels, liver, bones, and joints. At this stage, syphilis is usually no longer contagious.
Tertiary syphilitic gummas may mimic basal cell carcinoma. The gummatous tumors are benign and, if properly treated, in most cases will heal and the patient will recover.
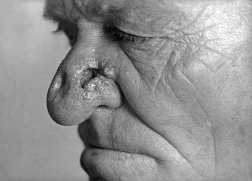
A photograph of a patient with tertiary syphilis resulting in gummas seen here on the nose. Photo Credit: CDC/ Susan Lindsley
This patient presented with a gumma of nose due to a long standing tertiary syphilitic Treponema pallidum infection.
Photo Credit: CDC/ J. Pledger

This patient presented with a swollen scrotum, which was diagnosed as a syphilitic gumma of the testicle.
Photo Credit: CDC/Susan Lindsley, VD
Condylomata lata
Condylomata lata lesions usually present as gray, raised papules that sometimes appear on the vulva or near the anus, or in any other warm intertriginous region.
Because this type of cutaneous lesion is also a symptom manifested by illnesses other than syphilis such as condylomata acuminata, a differential diagnosis must be performed in order to rule out other possibilities. Syphilis is known as the “great imitator” for, as in this case, manifestations often resemble other disease processes.

This patient presented with a case of secondary syphilis manifested as perianal wart-like growths.
Photo Credit: CDC

This patient presented with several infra-scrotal condylomatous lesions, which is one of the manifestations of secondary syphilis.
Photo Credit: CDC/ Susan Lindsley

This patient presented with secondary syphilitic lesions of vagina.
Photo Credit: CDC/ J. Pledger

This patient presented with a case of alopecia during the secondary stage of syphilis.
Photo Credit: CDC/ Susan Lindsley

This patient presented with a case of alopecia during the secondary stage of syphilis.
Photo Credit: CDC
Interstitial keratitis
Interstitial keratitis, which is an inflammation of the cornea’s connective tissue elements, and usually affects both eyes, can occur as a complication brought on by congenital, or acquired syphilis. IK usually occurs in children older than two years of age.
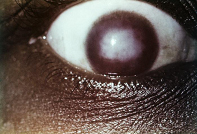
This photograph depicts the presence of a diffuse stromal haze in the cornea of a female patient, known as interstitial keratitis (IK), which was due to her late-staged congenital syphilitic condition.
Photo Credit: CDC/ Susan Lindsley, VD