Maternal Mortality
Governor Tim Walz proclaimed Jan. 23 as Maternal Health Awareness Day.
View the proclamation.
Minnesota Maternal Mortality Update Reporting for 2017-2019 (PDF)
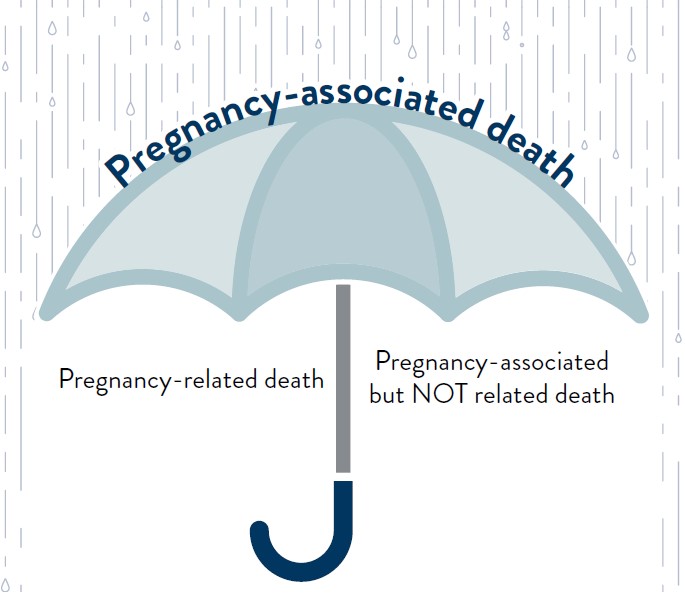
Maternal mortality definitions
In 1993, the Minnesota Department of Health (MDH) adopted the Center for Disease Control and Prevention (CDC) definition of maternal mortality:
- Pregnancy-associated death: A death during pregnancy or within one year of the end of pregnancy, irrespective of cause.
The following are subsets of pregnancy-associated maternal deaths:
- Pregnancy-related death: A death during pregnancy or within one year of the end of pregnancy from a pregnancy complication, a chain of events initiated by pregnancy, or the aggravation of an unrelated condition by the physiologic effects of pregnancy.
- Pregnancy-associated but NOT related death: A death during pregnancy or within one year of the end of pregnancy from a cause that is not related to pregnancy.
Maternal mortality in Minnesota
The Minnesota Department of Health’s maternal mortality review committee (MMRC) reviews cases of pregnancy-associated deaths of Minnesota residents. Pregnancy-associated death is a death that occurs during pregnancy or within one year after the end of a pregnancy irrespective of cause. The data and recommendations of the review committee can be found in Minnesota’s Maternal Mortality Report. This report includes demographic information and characteristics of pregnancy-associated deaths of Minnesotans and summarizes the leading causes and contributing factors of pregnancy-associated deaths.
Recommendations from review of pregnancy-associated deaths
The MMRC’s goal is to identify contributing factors and recommendations to prevent future deaths for the identified pregnancy-associated deaths. Key recommendations from reviewed deaths from 2017-2021 are:
- Integrate mental health support into prenatal and postpartum care, particularly for individuals with a history of mental illness, substance use disorders, or trauma. This includes direct referrals to mental health and substance use disorder services, providing early interventions, and ensuring that mental health concerns are addressed with the same level of priority as physical health issues. Integrate culturally responsive care that considers the diverse needs of various racial and ethnic groups, including Black and American Indian people. Health care systems should train staff on cultural humility (culturally-centered care) and implicit bias, integrate interpreters, and provide care that is respectful of cultural differences. Law enforcement should develop pathways to refer individuals in crisis to supportive services. Examples of crises include unhoused families, acute substance use effects in the perinatal population, and intimate partner violence.
- Provide robust follow-up and emotional, physical, and mental health support to families after pregnancy. There is an urgent call for postpartum doulas, home visitors, and other wraparound services to support the mental, emotional, and physical needs of new parents. Ensure the safety of all families during the perinatal period. Families need access to stable housing, childcare, transportation, and other basic needs, which are essential for improving health outcomes. Improve continuity and coordination of care.
- Advocate for policy changes that ensure comprehensive, accessible, and equitable care for all pregnant and postpartum individuals, especially those from marginalized communities.
To learn more, review recommendations found in the Minnesota Maternal Mortality Update Reporting for 2017-19 (PDF). Updated maternal mortality data from the Minnesota maternal mortality review is now available on pregnancy-associated deaths occurring from 2017-2021. This report brings together five years of case data and recommendations. The recommendations from the previous report are still applicable. The release of the new update adds more actionable recommendations for the state to address pregnancy-associated deaths.
- Minnesota Maternal Mortality Report: Reporting for 2017-2019 (PDF)
- Minnesota Maternal Mortality Report 2017-2018 (PDF)
- Recommendations from Review of 2017 Cases (PDF)
- Recommendations from Review of 2016 Cases (PDF)
Maternal mortality nationally
The Centers for Disease Control and Prevention (CDC) has many tools and resources regarding maternal mortality. CDC is committed to preventing pregnancy-related deaths and ensuring the best possible birth outcomes. Learn more by visiting Maternal Mortality Prevention.
The following reports from the CDC provide an overview of national maternal mortality data.
This report combines and shares data from a majority of U.S. States which were actively reviewing pregnancy-associated deaths from 2017-2019 using the maternal mortality review process. The report shares information about the preventability of maternal deaths along with nationwide demographics and circumstances.
This report is a focused evaluation of 36 states’ pregnancy mortality surveillance systems from 2017-2019, analyzing preventability and factors contributing to pregnancy-related deaths.
This report provides data about the differences in perinatal outcomes by racial group.
Minnesota maternal mortality review project
Per Minnesota Statute 145.901, “the commissioner of health may conduct maternal death studies to assist the planning, implementation, and evaluation of medical, health, and welfare service systems and to reduce the numbers of preventable maternal deaths in Minnesota.” To that end, the Minnesota maternal mortality review project was reinstituted in 2012 to review maternal deaths and examine the circumstances surrounding maternal deaths, identify risk factors for maternal mortality and make recommendations and interventions for reducing or eliminating future deaths in women of reproductive age.
The Minnesota maternal mortality review process
Step 1: Case findings
The Minnesota Department of Health (MDH) conducts surveillance of maternal deaths through standard and enhanced surveillance methods.
- Physician and hospital reporting
- Pregnancy status check box on death certificate
- ICD-10 codes
- Matching death certificates from any female death between the ages of 5-70 with birth certificates and/or fetal death certificates.
For more information on reporting deaths, see the Maternal Death Reporting Form (PDF).
Step 2: Assemble available medical records and information
Minnesota Statute 145.901 allows for the collection maternal medical records in accordance with the statute purpose. Decedent information is requested from multiple sources. Death certificates, birth certificates, medical records, autopsy reports, police reports and obituaries are some sources of information that are requested and collected. All available relevant medical records from a woman’s pregnancy, labor, birth, postpartum and other medical care are gathered to review the circumstances leading up to her death. The investigation of the maternal case aims to gain insight into the various factors (health, social, geographic, cultural, spiritual, psychological, environmental, economic, or other) that lead to the maternal death and to identify factors that may be preventable. This information is abstracted and developed into a case narrative, which is then reviewed by the Minnesota maternal mortality review committee.
Step 3: Minnesota maternal mortality review committee
The Minnesota Maternal Mortality Review Committee (MMRC) reviews all pregnancy-associated deaths occurring in Minnesota residents and is authorized in Minnesota Statutes 145.901. More information on the MMRC can be found on the MMRC webpage.
Step 4: Analysis
Maternal information is abstracted and analyzed in the Maternal mortality review information application (MMRIA). This application developed by the CDC, provides for a standardization of surveillance, information collection, and monitoring of maternal mortality rates, allowing states to detect similar trends.
Step 5: Use of recommendations
The recommendations from the Minnesota maternal mortality review project can be used to:
- Identify themes or trends in maternal mortality in Minnesota over time.
- Inform perinatal care providers and clinical practice and community stakeholders.
- Offer relevant public health interventions for women of reproductive age.
- Inform quality improvement projects and activities.
- Determine where resources should be allocated in the State.
- Influence policy at the state and local level.
Helpful resources
The following are national resources focused on maternal mortality:
- World Health Organization - Maternal Mortality
- Centers for Disease Control and Prevention Foundation
- Centers for Disease Control and Prevention - Maternal Mortality Prevention
- National Network of Perinatal Quality Collaborative
- Maternal Health Action & Resource Center (MHARC)
- Association of Maternal & Child Health Programs
- March of Dimes - It Starts With Mom
- March of Dimes Report Card
- Alliance for Innovation on Maternal Health Program