Contact Info
Clinical Recommendations for Patients with Underlying Medical Conditions: COVID-19
Patients who are older, who have one or more underlying medical conditions, or who are not up to date on COVID-19 vaccination are at increased risk of severe outcomes of COVID-19, such as hospitalization or death. Health care providers should consider a patient’s age, presence of underlying conditions, and other risk factors when determining the risk of severe COVID-19 outcomes for their patients.
High risk
Age
Age is the strongest risk factor for severe COVID-19 outcomes. That risk increases in people who are 50 years and older, with the risk increasing substantially at ages older than 65 years. Residents of long-term care facilities are also at increased risk of severe outcomes from COVID-19.
Race and ethnicity
People from racial and ethnic minority groups (American Indian or Alaska Native, Asian, Black or African-American, and Hispanic/Latino) have been disproportionately affected by the COVID-19 pandemic. CDC data (Health Disparities: Provisional Death Counts for COVID-19) has shown that, compared to non-Hispanic white people, people from these minority groups are more likely to be hospitalized and die from COVID-19 at younger ages.
Underlying medical conditions
Many underlying medical conditions have been associated with increased risk for severe COVID-19. Refer to CDC: Underlying Conditions and the Higher Risk for Severe COVID-19 for a more complete list. Key conditions include:
- Chronic heart, lung, kidney, and liver disease
- Diabetes
- Obesity (BMI >30 kg/m2 or >95th percentile in children)
- Disabilities
- Neurological conditions such as dementia
- Immunocompromising conditions or medications
- Pregnancy and recent pregnancy
- Smoking
- Children who are medically complex (e.g., who have neurologic, genetic, or metabolic disorders or congenital heart disease)
Vaccination status
Patients who are unvaccinated or who are not up to date with COVID-19 vaccines, including recommended boosters, are at increased risk for severe COVID-19 illness.
COVID-19 risk continuum
The risk of severe COVID-19 illness increases as the number of comorbid conditions and risk factors increases.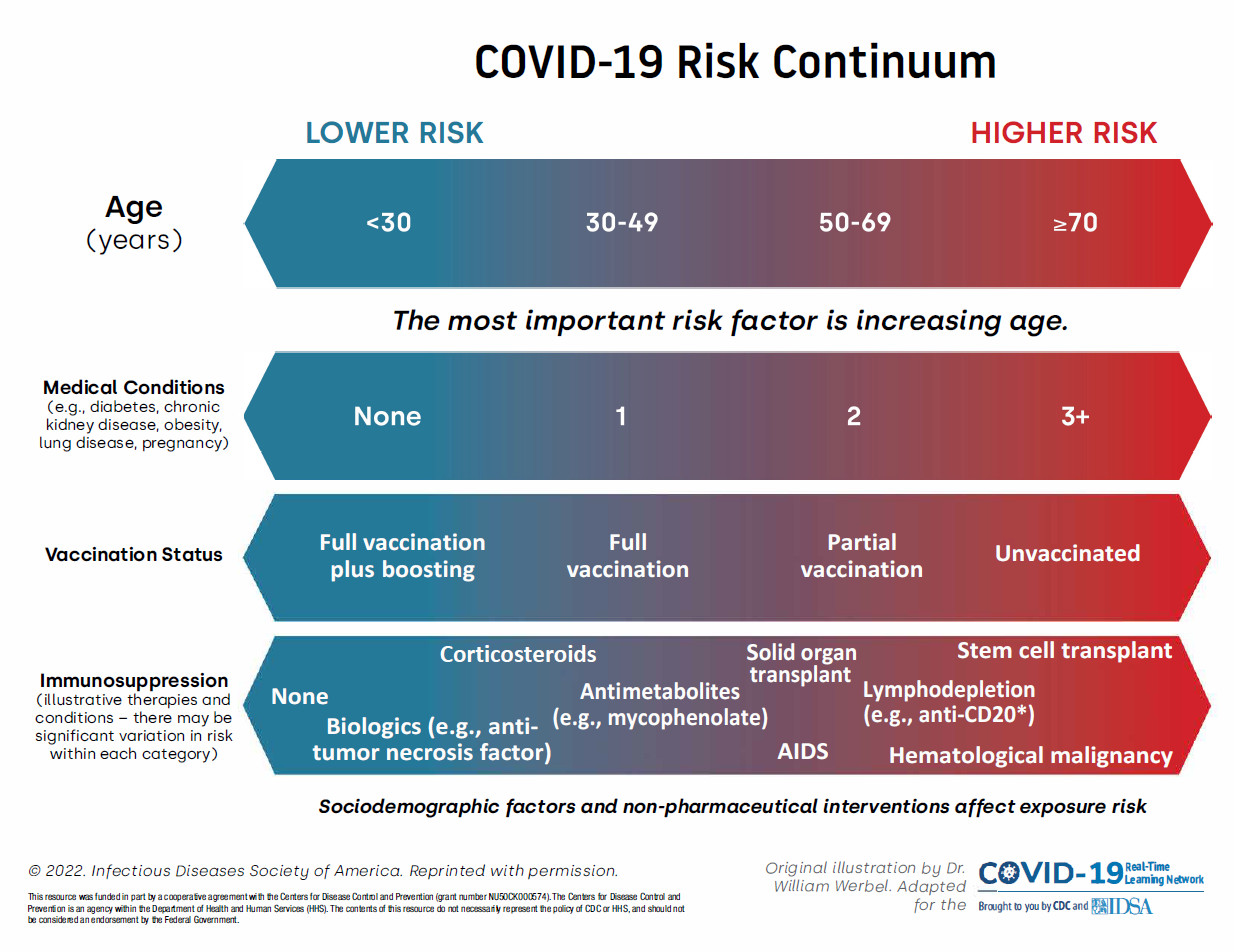
Figure 1: Risk for severe COVID-19 outcomes, represented along continua of several key modifiable and nonmodifiable risk factors. National Library of Medicine: Werbel WA, Weld ED, Advani SD, et al. Your Outpatient has Coronavirus Disease 2019: What Are the Treatment Options in the Current Severe Acute Respiratory Syndrome Coronavirus 2 Variant Climate? Clin Infect Dis. 2023, 77(1), 32–37. https://doi.org/10.1093/cid/ciad178.
Actions for health care providers
- Continue to recommend vaccination for COVID-19, including all recommended boosters.
- For clinical guidance and information on where to get vaccinated, refer to COVID-19 Vaccine.
- Consider antiviral therapies for patients with mild to moderate symptoms and underlying risk factors for severe illness.
- Eligibility is based on underlying risk, NOT severity of symptoms. Treatment must be started early to be effective.
- Visit Therapeutic Options for COVID-19 Patients for more information on therapeutic options (including pre-exposure prophylaxis for eligible patients) and prescribing.
- Encourage patients with underlying risk factors for severe illness to continue practicing preventive measures, such as when to wear a high-quality mask, to decrease the risk of infection.
- Patient information is available at Protect Yourself and Others.
- Encourage patients with underlying risk factors to have a COVID-19 plan in place, including testing at the first sign of symptoms and knowing how to access treatment if needed.