Commercial Tobacco Use
- Commercial Tobacco Use Home
- Data and Reports
- Get Help Quitting
- Prevention and Treatment
- Tobacco and Your Health
Learn More
- Behavioral Health and Commercial Tobacco
- E-cigarettes and Vaping
- Flavored Commercial Tobacco
- Menthol Commercial Tobacco
- Nicotine and Nicotine Dependence
- Nicotine Pouches and Other Emerging Products
- Promoting Quitting and Treatment
- Secondhand Smoke and Aerosol
- Smoke-Free Housing
- Traditional and Sacred Tobacco
Related Topics
Contact Info
Behavioral Health and Tobacco Use in Minnesota
Despite overall declines in adult cigarette use, some populations still smoke at higher rates, including people with behavioral health issues such as mental illness and substance use disorders. For people in substance abuse treatment, quitting can increase long-term abstinence from alcohol and other drugs.1
Smoking is higher among Minnesotans with behavioral health issues.
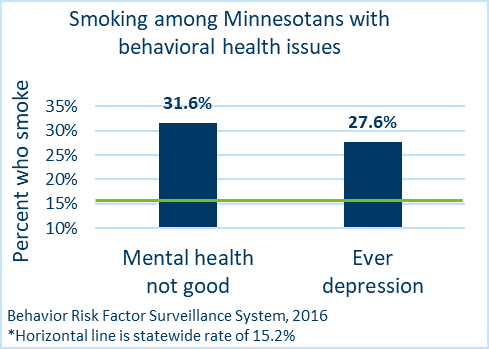 Smoking rates are higher for Minnesota adults with depression and serious psychological distress, and adults who are currently taking medications or receiving treatment for mental or emotional health problems.2
Smoking rates are higher for Minnesota adults with depression and serious psychological distress, and adults who are currently taking medications or receiving treatment for mental or emotional health problems.2
Minnesotans with psychological distress smoke at more than twice the overall statewide rate.2
Tobacco-related death and disease is higher among smokers with behavioral health issues.3, 4
Nationally, people with mental illness die about 10 years earlier than those without mental illness,5 and half of smoking-related deaths each year (200,000) are among people with mental illnesses.6
Compared to people without serious mental illness, Minnesota adults with serious mental illness and a tobacco-related disease die approximately 32 years sooner.7
Quitting can improve the success of addiction treatment.
People with behavioral health issues are interested in quitting, can quit, and benefit from quitting.8-13 Quitting smoking more than doubles the likelihood of successful treatment for substance abuse.14
However, people with mental illness may face challenges in quitting and need additional counseling and longer use of smoking cessation medications. In-person or telephone counseling and smoking cessation medications, including nicotine replacement therapies, greatly improve the chances that a person will be successful in their quit attempt.15, 16
Free quitting help is available to all Minnesotans. Quit Partner (1-800-QUIT-NOW [784-8669]) offers a variety of tools, including coaching, quit guides, and starter kits with patches, gum, or lozenges. Minnesota residents with Medical Assistance or MinnesotaCare also have free access to tobacco cessation counseling and medications with a prescription.
Learn more about Quitting Tobacco.
Communities can help reduce tobacco use among people with behavioral health issues.
Efforts to reduce tobacco use among people with behavioral health issues include policy strategies to increase tobacco-free environments and encourage cessation. The Minnesota Comprehensive Tobacco Control Framework 2022-2026) states that helping individuals break free from tobacco addiction requires multiple levels of intervention, including developing and implementing strategies to integrate tobacco dependence treatment within mental illness and substance use disorder treatment.
Change norms around tobacco treatment for people with behavioral health issues.
It is important to engage behavioral health professionals and raise awareness of the harms of nicotine addiction and tobacco use, as well as the benefits of tobacco treatment.
Integrate tobacco screening and treatment referral.
Providers should ask, advise and provide treatment or refer people interested in quitting to tobacco cessation resources. A tobacco cessation counselor can assist individuals in quitting. Tobacco cessation resources and services are available to help people quit using tobacco.
Implement comprehensive tobacco-free grounds policies.
In Minnesota, mental health and substance use facilities are adopting tobacco-free grounds policies and encouraging quitting among both clients, staff, and visitors. In 2018, three large behavioral (or mental) health facilities will go smoke free, protecting over 40,000 clients from secondhand smoke exposure.
Download this information: Behavioral Health and Tobacco Use in Minnesota (PDF)
Learn more
- Quitting Commercial Tobacco - Information about Minnesota's free quit support programs.
- Helping People Quit - More resources for organizations or individuals working with people who use commercial tobacco.
- Mental Health Promotion
- Lung Mind Alliance - The Lung Mind Alliance is a statewide coalition with the goal of reducing disparities related to the impact of commercial tobacco on people with mental illness and/or substance use disorders
- Behavioral Health (Smoking Cessation Leadership Center)
- National Behavioral Health Network for Tobacco and Cancer Control
References
- Weinberger, A.H., et al., Cigarette Smoking Is Associated With Increased Risk of Substance Use Disorder Relapse: A Nationally Representative, Prospective Longitudinal Investigation. The Journal of clinical psychiatry, 2017. 78(2): p. e152.
- Centers for Disease Control and Prevention, Behavioral Risk Factor Surveillance System. 2013.
- Bandiera, F.C., et al., Tobacco-related mortality among persons with mental health and substance abuse problems. PloS one, 2015. 10(3): p. e0120581.
- Callaghan, R.C., et al., Patterns of tobacco-related mortality among individuals diagnosed with schizophrenia, bipolar disorder, or depression. Journal of psychiatric research, 2014. 48(1): p. 102-110.
- Walker, E.R., R.E. McGee, and B.G. Druss, Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry, 2015. 72(4): p. 334-341.
- Grant, B.F., et al., Nicotine dependence and psychiatric disorders in the united states: Results from the national epidemiologic survey on alcohol and relatedconditions. Archives of general psychiatry, 2004. 61(11): p. 1107-1115.
- Minnesota Health Care Programs (MHCP) Client Data, M.D.o.H. Services, Editor. 2008-2012.
- Siru, R., G.K. Hulse, and R.J. Tait, Assessing motivation to quit smoking in people with mental illness: a review. Addiction, 2009. 104(5): p. 719-733.
- Lukowski, A.V., et al., Quitline outcomes for smokers in 6 states: rates of successful quitting vary by mental health status. Nicotine & Tobacco Research, 2015. 17(8): p. 924-930.
- Dickerson, F., et al., Smoking cessation in persons with serious mental illnesses: The experience of successful quitters. Psychiatric Rehabilitation Journal, 2011. 34(4): p. 311-316.
- Peckham, E., et al., Exploring why people with SMI smoke and why they may want to quit: baseline data from the SCIMITAR RCT. Journal of psychiatric and mental health nursing, 2016. 23(5): p. 282-289.
- Taylor, G., et al., Change in mental health after smoking cessation: systematic review and meta-analysis. Bmj, 2014. 348: p. g1151.
- McKelvey, K., J. Thrul, and D. Ramo, Impact of quitting smoking and smoking cessation treatment on substance use outcomes: An updated and narrative review. Addictive behaviors, 2017. 65: p. 161-170.
- Tsoh, J.Y., et al., Stopping smoking during first year of substance use treatment predicted 9-year alcohol and drug treatment outcomes. Drug and alcohol dependence, 2011. 114(2): p. 110-118.
- Roberts, E., et al., Efficacy and tolerability of pharmacotherapy for smoking cessation in adults with serious mental illness: a systematic review and network meta‐analysis. Addiction, 2016. 111(4): p. 599-612.
- Rogers, E.S., et al., Telephone smoking-cessation counseling for smokers in mental health clinics: a patient-randomized controlled trial. American journal of preventive medicine, 2016. 50(4): p. 518-527.
